Research Article | DOI: https://doi.org/10.31579/2835-9216/001
Research Article: Right ventricle Outflow Tract Acceleration Time: Correlation with Left Ventricular Diastolic Function
- Liz Andréa Villela Baroncini *
- Kenia Urnau
- Ana Cristina Camarozano
- Daniela de Castro Carmo
- Jerônimo Antonio Fortunato
- Rubens Zenóbio Darwich
Red Cross Hospital – Brazilian Red Cross – Paraná State Branch and Saber e Aprender Institute – Specialization Course in Transthoracic Echocardiography.
*Corresponding Author: Liz Andréa V Baroncini, Hospital da Cruz Vermelha – Cruz Vermelha Brasileira- Filial do Estado do Paraná e Instituto Saber e Aprender – Curso de Especialização em Ecocardiografia Transtorácica, Brazil.
Citation: Liz Andréa Villela Baroncini, Kenia Urnau, Ana Cristina Camarozano, Daniela de Castro Carmo, Jerônimo Antonio Fortunato, et al., (2022). Research Article: Right ventricle Outflow Tract Acceleration Time: Correlation with Left Ventricular Diastolic Function, Carcinogenesis and Chemotherapy, 1(1); Doi: 10.31579/2835-9216/001
Copyright: © 2022, Liz Andréa Villela Baroncini. This is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 09 September 2022 | Accepted: 15 September 2022 | Published: 21 September 2022
Keywords: diastole; doppler echocardiography; left ventricular dysfunction; pulmonary artery
Abstract
Background: There is no available data about the measurement of acceleration time at the right ventricle outflow tract (AcT) and its relevance in the analysis of the left ventricular diastolic function (LVDF).
Objective: To correlate AcT with echocardiographic parameters of LVDF.
Method: Eighty-seven patients (58.4±14.5 years; 52% women) submitted to transthoracic echocardiogram assessing spectral and tissue Doppler of the transmitral flow and mitral annulus, AcT, left atrial volume (LAV), and pulmonary artery systolic pressure (PASP). Patients with systolic dysfunction of the LV and grades II and III diastolic dysfunction (DD) were excluded. Main analyses were performed using the Spearman’s Correlation Coefficient (SCC) and Pearson’s Linear Correlation Coefficient (PLCC).
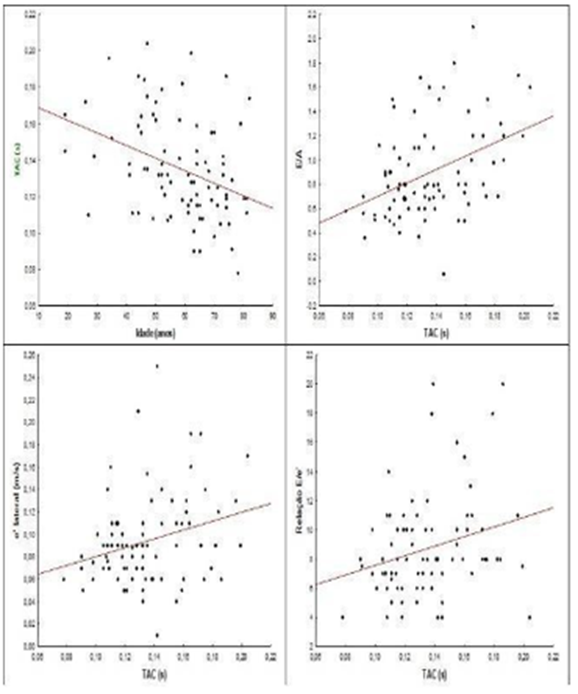
Results: A negative correlation between AcT value and age (PLCC – 0.36; Student’s t-test; p <0.001) and a positive correlation between AcT and E/A ratio (SCC 0.38; p<0.001), between AcT and E/e’ ratio (SCC 0.26; p=0.01), between AcT and E wave of the mitral flow (PLCC 0.36; p= 0.001) were found. LAV and PASP did not correlate with AcT. In patients with a normal diastolic function, AcT was higher when compared with the AcT in patients with Grade I DD (0.150±0.029ms versus 0.127±0.023ms; p<0.001; Student’s t-test). The threshold suggested in this subgroup of patients was 0.135s.
Conclusions: The present study correlated, unprecedentedly, AcT with echocardiographic parameters of the LV diastolic function. AcT values lower than 0.135s were associated with grade I diastolic dysfunction and higher than 0.135s values were associated with normal diastole.
Introduction
Diastole is a complex process of the cardiac cycle, dependent on the active myocardial relaxation, ventricular compliance, ventricular synchrony, ventricular diastolic suction, myocardial viscoelasticity, atrial contraction, pericardial restriction, interaction between right ventricle (RV) and left ventricle (LV) and the erectile function of the coronary arteries [1]. An altered RV-LV interaction leads to a diastolic dysfunction characterized by an increased dependence of the left ventricle filling in relation to the left atrial contraction [2]. Additionally, the diastolic function is affected by clinical factors such as age, systemic arterial hypertension and pulmonary arterial hypertension [3-4].
In this regard, at the transthoracic echocardiography (TTE), the assessment of the left ventricle diastolic function (LVDD) must be performed by integrating several techniques including the analysis of the spectral Doppler of the mitral flow, the tissue Doppler of the mitral annulus, pulmonary veins flow, the estimates of the pulmonary artery systolic pressure (PASP) and of the left atrial volume (LAV)[1]. PASP is most commonly determined by estimating the peak tricuspid regurgitant velocity, not always present, by means of the continuous wave Dopplerp [5], adding the right atrial pressure by assessing the inferior vena cava. An alternate option to estimate the pulmonary arterial pressure is to measure the right ventricle outflow tract acceleration time (AcT), which presented high correlation with PASP in previous studies, with a reference
value of 105ms [5-7]. Nevertheless, there are no published studies correlating its value with the conventional variables of the LV diastolic function assessed at TTE. Hence, the present study seeks to correlate AcT with the traditionally used variables at ETT to assess the LVDD, among them, E and A waves, E/A ratio, and isovolumetric relaxation time (IVRT) trough spectral Doppler of the mitral flow, septal and lateral e’ waves at tissue Doppler of the mitral annulus, E/e´ ratio (E/mean between septal and lateral e’), LAV and PASP.
Methods
This observational and transversal study includes 94 patients, from both genders, any ethnic background, over 18 years of age, from an outpatient cardiology unit of a public hospital, recommended by the assistant physician to undergo transthoracic echocardiogram for any clinical indication. The patients’ selection did not follow any statistical criterion, but that of convenience, that is, according to their availability to participate in the research study. For each patient, a protocol form with clinical and echocardiographic parameters was completed. Analyzed demographic data included age, gender, body mass index (BMI), presence of hypertension, diabetes mellitus (DM), dyslipidemia, coronary arterial disease (CAD), history of current or former smoking, and frequent or continuous use of prescribed drugs. Diagnoses for hypertension, DM,
yslipidemia, and CAD were recorded in the patients’ medical files and/or reported by the patients themselves (referral information data).
Patients underwent a complete bidimensional transthoracic echocardiogram with the Phillips IE 33, Envisor or Vivid E General Electric models. In all acoustic views, all standard measurements and echocardiographic analyses were conducted in each patient and the sonographic analyses were performed by two experienced echocardiographers, holders of echocardiography certificates from the Cardiovascular Imaging Department of the Brazilian Society of Cardiology.
Exclusion criteria included patients with (a) significant valvular heart disease (moderate and severe); (b) prosthetic heart valves; (c) pulmonary emphysema or chronic obstructive pulmonary disease; (d) moderate to severe pulmonary arterial hypertension (PASP > 50 mmHg); (e)atrial fibrillation or pacemaker rhythm; f) dilated cardiomyopathy or ischemic cardiomyopathy with regional wall motion abnormality or myocardial segmental thickness of left ventricle; (g) LV systolic dysfunction (ejection fraction <52>
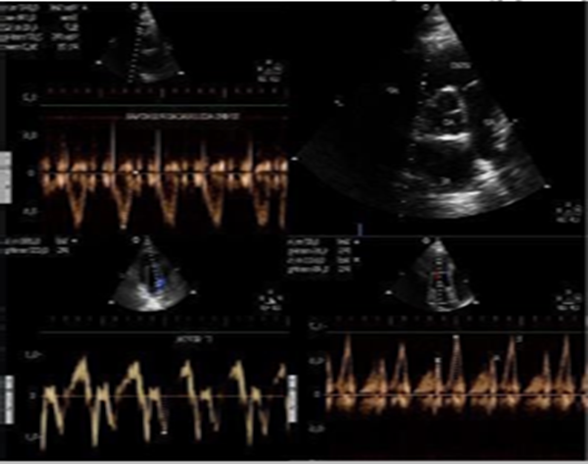
In this study, the main echocardiographic variables assessed were: (a) at the transmitral spectral Doppler, the E wave velocity, A wave velocity, E/A ratio and isovolumetric relaxation time (IVRT); (b) from the mitral annular tissue Doppler imaging, septal e’ wave velocity, lateral e’ wave velocity, mean velocity between septal e’ and lateral e’; (c) E/e’ ratio (E wave velocity/mean velocity between septal e’ and lateral e’); (d) acceleration time at the right ventricle outflow tract (AcT), measured on the short axis view toward the heart base vessels, at the tip of the pulmonary valve leaflet, from the start to the peak of the systolic flow; (e) left atrial volume (LAV) and (f) pulmonary artery systolic pressure (PASP), measured by the tricuspid regurgitation peak velocity, when present (Figures 1 and 2)
Statistical Analysis
The results obtained were described by means, medians, minimum and maximum values, and standard deviations (quantitative variables) or by frequencies and percentages (categorical variables). To assess the association between two quantitative variables, Pearson’s or Spearman's linear correlation coefficient was used. The comparison of two groups in relation to the quantitative variables was performed by the student's' t test for independent samples. The one-way analysis of variance (ANOVA) was used to compare more than two groups. The Kolmogorov- Smirnov normality test examined whether the variables were normally distributed. Values of p<0>
Results
Seven patients, out of the 94 initially selected, were excluded from the study. Final analysis included 87 patients, 58.4±14.5 years; 45 (52%) women. Clinical characteristics of the studied cohort are listed in Table 1.
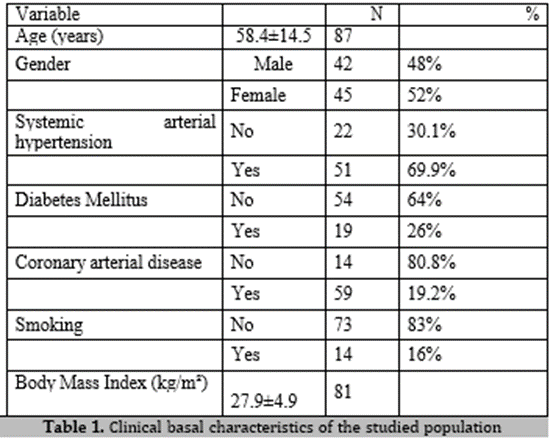
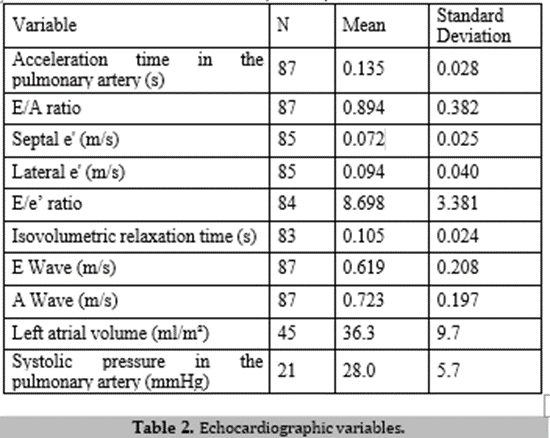
Values from the identified echocardiographic variables corroborate those values from the available literature (Table 2).
A negative and significant correlation (Spearman’s correlation coefficient (SCC) between AcT value and age (SCC – 0.36; p = 0.001) and a tendency between AcT value and wave A (SCC -0.21; p = 0.05) were observed. Additionally, positive and significant correlations were identified between AcT value and E/A ratio (SCC 0.38; p=<0 p=0.04), p=0.01) xss=removed>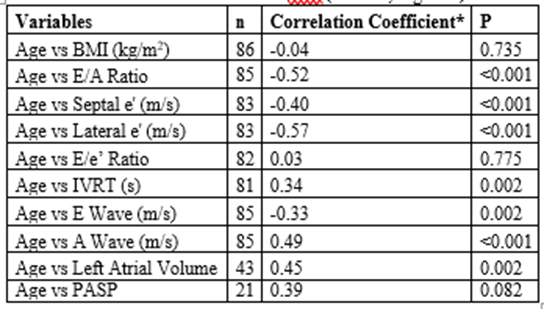
Discussion
The present study presented unprecedent correlation of AcT absolute values with echocardiographic variables representatives of LV diastolic function. Concomitantly, the same values have shown to change with age increase. Previous studies report that LV diastolic function changes and progresses with age[11-12], independent of a LV preserved systolic function, and may even lead to heart failure with normal LV ejection fraction[13-15]. Similarly, the systolic pressure in the pulmonary artery progressively increases with age both at rest and during exercise[16-17]. AcT values identified in this study follow the same alterations. The rigid exclusion criteria applied enabled the assessment of the LV diastolic function and AcT without the influence of other factors, such as the presence of a significant pulmonary arterial hypertension, systolic dysfunction or advanced grades of LV diastolic dysfunction, which might lead to different interpretations. These same criteria determined homogeneity in the studied cohort. Hence, it was possible to observe that correlation of E/A ratio at mitral spectral Doppler decreases with age (following the decrease of wave E velocity and increase of A wave). Values of septal and lateral e’ waves of the mitral annulus at tissue Doppler also decreased. These findings corroborate former studies involving a larger cohort of patients[18-19]. Similarly, AcT values followed the same values obtained for the LV diastolic function variables used in this study: the age increase correlated with AcT lower values, the lower AcT values correlated significantly with lower values of the E/A ratio, with lower values of E and lateral e’ waves. However, E/e’ ratio presented a positive correlation with AcT value, specifically, lower AcT values correlated with lower values of the E/e’ ratio. This finding may be accounted for by analyzing the behavior of lateral and septal e’ waves that decrease with age (about 10 to 15 years earlier) when compared with E wave of spectral Doppler, which decreases at a late stage, as described by Kadappu KK et al. In the present study, a stronger negative correlation of age with septal and lateral e’ waves in relation to E wave of the spectral Doppler was observed. Hence, in an early stage of the diastolic dysfunction, without the increase of the filling pressures of the left atrium (LA), the E/e’ ratio is still low, as is the AcT value, since e’ waves decrease more sharply than E wave in this phase. Similar explanation is provided for the lack of correlation between IVRT and Act values. It is known that IVRT prolongs with age; however, when there is an increase in the filling pressures, IVRT shortens21. The selected severe exclusion criteria also enabled assessment of AcT in quasi-normality conditions. PASP mean value was 28mmHg and its maximum value was 40mmHg, values considered to be within normality for the age range in the studied population[22]. Hence, a correspondence between AcT and PASP would only be expected in the presence of significant pulmonary hypertension, which was not the purpose of this study. However, when patients with a normal LV diastolic function and those with grade I diastolic dysfunction were compared, the latter presented lower AcT values, suggesting an increase in the pulmonary arterial pressure in this group, although still within their normal values. AcT values below 105ms are considered abnormal or reveal an increase in the pulmonary arterial pressure (PAH) [23]. Conversely, by excluding patients with a significant pulmonary arterial hypertension from the studied cohort, AcT values below 105ms were not expected. However, in an unprecedent way, it was possible to identify an alteration in AcT value in patients without a significant PAH, with an initial alteration of the LV diastolic function when compared with a preserved LV diastolic function. Some limitations of this study include the small number of participants, lack of data about the size and function of the right chambers and lack of analysis of the intra- and inter-observer measurement variability in relation to AcT, as errors may occur, considering that AcT values are affected by heart rates, cardiac output, RV systolic function and technical difficulties such as the angle of the ultrasonic beam[5].
Conclusions
The present study correlated significantly and unprecedentedly AcT with echocardiographic parameters of the LV diastolic function, presenting lower values in individuals with grade I diastolic dysfunction. The threshold suggested by the ROC curve was 0.135s, with AcT values lower than 0.135s associated with grade I diastolic dysfunction and higher than 0.135s values associated with normal diastole.
References
- Diretrizes das indicações da Ecocardiografia. Avaliação da função e estrutura ventricular esquerda. Sociedade Brasileira de Ecocardiografia. Arq Bras Cardiol 2009; 93(supl.3):e265-e266.
View at Publisher | View at Google Scholar - Bossone E, D’Andrea A, D’Alto M, Citro R, Argiento P, et al (2013).Echocardiography in pulmonar artery hypertension: from diagnosis to prognosis. J Am Soc, Echocardiogr;26:1-14.
View at Publisher | View at Google Scholar - Mitter SS, Shah SJ, Thomas JD.(2017). A test in context. E/A and E/e’ to asses diastolic dysfunction and LV filling pressure. J Am Coll Cardiol;69(1):1451-1464.
View at Publisher | View at Google Scholar - Rosa EC, Moysés VA, Rivera I, Sesso RC, Kohlmann N, et al (2002). Left ventricular diastolic function in essential hypertensive patients. Influence of age and left ventricular geometry. Arq Bras Cardiol;78:472-477.
View at Publisher | View at Google Scholar - Yared K, Noseworthy P, Weyman AE, McCabe E, Picard MH, et al (2011). Pulmonary artery acceleration time provides an accurate estimate of systolic pulmonary arterial pressure during transthoracic echocardiography. J Am Soc Echocardiogr;24:687- 692.
View at Publisher | View at Google Scholar - Lopez-Candales A, Eleswarapu A, Shaver J, Edelman K, Gulyasy B, et al(2010). Right ventricular outflow tract spectral signal: a useful marker of right ventricular systolic performance and pulmonary hypertension severity. Eur J Echocardiogr;11:509-515.
View at Publisher | View at Google Scholar - Grapsa J, Tzemos N.( 2018). Echocardiography in pulmonary hypertension: current evidence and future perspectives. Continuing Cardiology Education;3:4.
View at Publisher | View at Google Scholar - Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, et al (2015). Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr;28:1-39 e14.
View at Publisher | View at Google Scholar - DiLorenzo MP, Bahtt SM, Mercer-Rosa L.(2015). How best to assess right ventricular function by echocardiography. Cardiol Young;25:1473-1481.
View at Publisher | View at Google Scholar - Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher et al (2010) . Diretrizes para avaliação ecocardiográfica do coração direito em adultos: um informe da Sociedade Americana de Ecocardiografia. Aprovado pela Associação Européia de Ecocardiografia (registrada pela Sociedade Européia de Cardiologia), e pela Sociedade Canadense de Ecocardiografia. J Am Soc Echocardiogr;23:685-713.
View at Publisher | View at Google Scholar - Campbell DJ, Somaratne JB, Jenkins AJ, Prior DL, Yii et al (2012) Diastolic dysfunction of aging is independent of myocardial structure but associated with plasma advanced glycation end- product levels. PLoS ONE;7(11):e49813.
View at Publisher | View at Google Scholar - Carvalho JC, Farand P, Do HD, Brochu MC, Bonenfant F, et al (2013). Effect of age and sex on echocardiographic left ventricular diastolic function parameters in patients with preserved ejection fraction and normal valvular function. Cardiol J;20:513-518.
View at Publisher | View at Google Scholar - Garvan C. Kane, Barry L. Karon, Douglas W. Mahoney, Margaret M. Redfield, Veronique L. Roger. et al (2011). Progression of Left Ventricular Diastolic Dysfunction and Risk of Heart Failure. American Medical Association;8;24-31.
View at Publisher | View at Google Scholar - Aziz F, TK LA, Enweluzo C, Dutta S, Zaeem M. (2013). Diastolic heart failure: a concise review. J Clin Med Res;5:327-334.
View at Publisher | View at Google Scholar - Zakeri R, Cowie MR. (2018).Heart failure with preserved ejection fraction: controversies, challenges and future directions. Heart;0:1- 8.
View at Publisher | View at Google Scholar - Kane GC, Sachdev A, Villarraga HR, Ammash NM, Oh JK, et al (2016).Impact of age on pulmonary artery systolic pressures at rest and with exercise. Echo Res Pract;3:53-61.
View at Publisher | View at Google Scholar - Mahjoub H, Levy F, Cassol M, Meimoun P, Peltier M, et al (2009). Effects of age on pulmonary artery pressure at rest and during exercise in normal adults. Eur J Echo;10:635-640.
View at Publisher | View at Google Scholar - Parick JD, Hollignsworth KG, Wallace D, Biamire AM, MacGowan GA. (2016) Normal Age-related changes in left ventricular function: Role of after load and subendocardial dysfunction. Intern J Cardiol;223;306-312.
View at Publisher | View at Google Scholar - Studart PCC, Belém LHJ, Rabischoffisk A, Nogueira AC. (2006). The tissue doppler in the evaluation of the left ventricle diastolic function: its value in the detection of the early alterations and the understanding of the evolution of the dysfunction with normal systolic function. Rev SOCERJ;19:232-238.
View at Publisher | View at Google Scholar - Kadappu KK, Thomas L. (2015).Tissue Doppler imaging in echocardiography: value and limitations. Heart, Lung and Circulation;24:224-233.
View at Publisher | View at Google Scholar - Zhang W, Kovács SJ (2009). The age dependence of left ventricular filling efficiency. Ultrasound Med Biol;35:1076-1085.
View at Publisher | View at Google Scholar - Granstam S-O, Björklund E, Wikström G, Roos MW (2013). Use of echocardiographic pulmonary acceleration time and estimated vascular resistance for the evaluation of possible pulmonary hypertension. Cardiovascular Ultrasound; 11:17. Marra AM, Benjamin N, Ferrara F, Vriz O, D’Alto M, et al (2017). Reference ranges and determinants of right ventricle outflow tract acceleration time in healthy adults by two-dimensional echocardiography. 33(2):219-22
View at Publisher | View at Google Scholar

 Clinic
Clinic
