Research Article | DOI: https://doi.org/10.31579/2834-5029/027
Prevalence of Intestinal Stoma Complications and Associated Factors Among Children in Uganda, A Cross Sectional Study
1 Makerere University, Wandegeya, Makerere, Kampala, Uganda.
2 Mulago National Specialized Hospital, Mulago, Kampala, Uganda.
*Corresponding Author: Godfrey Kimbugwe, Makerere University, Wandegeya, Makerere, Kampala, Uganda.
Citation: Kimbugwe G., Kakembo N., Kisa P., Okeny P., Sekabira J., (2023), Prevalence of Intestinal Stoma Complications and Associated Factors Among Children in Uganda, A Cross Sectional Study, International Journal of Biomed Research, 2(3): DOI:10.31579/2834-5029/027
Copyright: © 2023, Godfrey Kimbugwe. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 10 July 2023 | Accepted: 08 August 2023 | Published: 16 August 2023
Keywords: cerebrovascular disease; ischemic stroke; hemorrhagic stroke; transient ischemic attack (TIA); high blood pressure; smoking
Abstract
Background: Intestinal stomas are a common procedure performed in children. They carry a high complication rate which affects the child, family and hospital. This study was aimed at documenting these complications and their associated factors.
Materials and Methods: This was a cross-sectional study carried out at the paediatric surgery unit of Mulago Hospital which is the main referral hospital in Uganda over a period of one and a half months. It included 131 children whose caretakers were interviewed and children physically assessed for presence of intestinal stoma complications.
Results: The mean age was 2 years (SD±1) with a male to female ratio of 1.3:1. Anorectal malformation (ARM) (77/131) was the most common indication for stoma formation followed by Hirschsprungs disease (25/131). Sigmoid colon was the most exteriorized part (104/131) followed by ileum (27/131). Children with intestinal stomas who developed complications were 83/131 with peristomal dermatitis being the most common complication (54/131) followed by stoma prolapse (5/131). The factors associated with intestinal stoma complications were stoma placement after the age of 12 months (OR 10.7, CI 1.47-17.62, p-value 0.019) and exteriorization of the ileum (CI 0-0.66, p-value 0.028).
Conclusion: The prevalence of intestinal stoma complications is high in Uganda with stoma placement after the age of one year and having an ileostomy as the associated factors. Sigmoid divided colostomies and prioritization of children with ileostomies for stoma reversal will help to significantly reduce intestinal stoma complications.
Introduction
Worldwide, intestinal stomas in children are temporarily placed mainly for congenital anomalies (73–87%) and a few acquired conditions (13–27%) to divert fecal stream, decompress bowel, protect gut anastomosis or a combination of these factors [1–3]. In Uganda, intestinal stomas are still one of the commonest procedures performed in the paediatric population [4].
Despite being lifesaving procedures, intestinal stomas carry with them significant morbidity and mortality especially stemming from the high rates of associated complications [5, 6]. These complications range from 28–74% worldwide [7, 8] and 30-81.7% in Africa [3, 9].
When complications arise, the management of children with intestinal stomas becomes more demanding. They need more resources both from parents and the hospital and lose more time through readmissions and hospital visits in addition to the definitive surgery and stoma reversal that they require. Sometimes emergency surgery has to be performed to deal with the complications which interferes with the hospital workflow and further increases the risk of complications for the patients [10].
Data from the national referral hospital show that over 98% of children wait between 6 months and 5 years to have their stomas reversed, a period during which complications increase and unfortunately children have to live with these complications for the same long periods [4, 11].
Factors that appear to increase the rate of intestinal stoma complications like absence of preoperative markings, height of the stoma, emergent stoma formation, lack of proper surgical technique, end stomas, loop stomas, inappropriate location and being placed by junior doctors are modifiable and hence can be dealt with to reduce complications [7, 12–14].
Despite the high number of stomas placed in children and the delay in reversal, the prevalence of intestinal stoma related complications and their associated factors in our setting is not known. Knowing these may help to formulate policies aimed at reducing stoma complications and improving the quality of life of these children. We therefore aimed to determine the prevalence of intestinal stoma complications in children and their associated factors in Uganda.
Materials and Methods
We conducted a cross sectional study at the paediatric surgery unit of Mulago National Referral Hospital (MNRH) to determine the prevalence and factors associated with stoma related complications among children aged below 12 years. MNRH is the national referral hospital for paediatric surgery patients in the republic of Uganda and is located in the capital city, Kampala.
The Paediatric Surgery unit is currently located in new Mulago ward 5B and admits children from birth to 12 years of age from different parts of Uganda through the accident and emergency unit, paediatric surgery outpatient clinic and paediatric medical wards. The unit is run by 7 paediatric surgeons, 4 fellows, 3 postgraduate students, 2 intern doctors and a team of 16 nurses. Daily surgeries are carried out by the team in the main operating theatre of the hospital, kids OR and the emergency theater.
We included 131 children with intestinal stomas placed at MNRH at least 1 month before the study started. We calculated the sample size using the Kish Leslie formula for proportions and Fleiss formula for comparing 2 proportions in a cross-sectional study. We excluded children with intestinal stomas placed from other hospitals because we could not determine associated factors in those hospitals and those with documented connective tissue disorders like prune belly syndrome who have been reported in literature to have an increased rate of complications like stoma prolapse. Consecutive sampling method was used.
Children at MNRH in the paediatric surgery ward and paediatric surgery outpatient department (PSOPD) with intestinal stomas were assessed. In addition, we used ward records to identify children with intestinal stomas and used telephone calls to invite their parents/guardians to the PSOPD or paediatric surgery ward to participate in the study.
Recruitment was done every day of the week on the paediatric surgery ward and every Wednesday in the PSOPD, which operates once a week. Informed consent was obtained from guardians of these children and assent from children 8 years and above and a structured interviewer-administered questionnaire was administered by the principal investigator or a trained research assistant to caretakers of recruited children. Please see Appendix 1 for the questionnaire used during the study.
We then physically assessed the recruited children for presence of intestinal stoma complications including peristomal dermatitis, retraction, prolapse, stenosis, necrosis, parastomal hernia, intestinal obstruction and malnutrition (WHO Z-score). We reviewed the unit`s operative logbook to assess and confirm some of the patient’s data.
Data were cleaned and transferred to STATA version 17.0 (Stata Corp) for analysis. Chi square test and corresponding p-values were used to compare participants with stoma complications and those without. Bivariate analysis was done using logistic regression and this was fitted to get crude odds ratios (OR). All independent variables with a p-value of <0>10% change in the adjusted and crude ORs for each variable. The level of significance was assessed at 95% confidence interval and P-Value of less or equal to 0.05. A parsimonious model with the highest and non-statistically significant R^2 test was considered.
Compliance with ethical standards
Ethical permission was obtained prior to commencement of the study from the department of Surgery, Mulago National Referral and Teaching Hospital and School of Medicine research and ethics committee of the College of Health Sciences, Makerere University. Written informed consent was obtained from parents/caretakers of children with intestinal stomas and assent was sought from children 8 years and above with intestinal stomas that were eligible for the study. All data obtained from the study was confidentially kept in password protected computers with only study investigators having access. Study identification numbers were used instead of children’s names.
Results
One hundred and thirty-one participants were analysed with a mean age of 2 years (SD±1) and majority 73 (55.7%) were males with a male to female ratio of 1.3:1. Most of our patients 70 (53.4%) were residing in nearby places and had care takers of primary education status 68 (51.9%). These were being taken care of by their mothers 124 (94.7%) and 106 (80.9%) had family earnings below 500,000/=UGX (approximately 131USD) per month as shown in table 1.
Characteristic | Frequency | Proportion | Exteriorized part | Frequency | Proportion |
Current age | Ileostomy | 27 | 20.6 | ||
1-12 months | 62 | 47.3 | Colostomy | 104 | 79.4 |
12-36 months | 13 | 9.9 | Type of stoma | ||
>36 months | 56 | 42.8 | Divided | 129 | 98.5 |
Sex | End | 2 | 1.5 | ||
Male | 73 | 55.7 | Cadre of the surgeon | ||
Female | 58 | 44.3 | Resident | 86 | 65.7 |
Residence | Fellow | 38 | 29 | ||
nearby | 70 | 53.4 | Surgeon | 7 | 5.3 |
surrounding districts | 16 | 12.2 | Theatre used | ||
Far districts | 45 | 34.4 | Casualty | 48 | 36.6 |
Attendant relationship | Main | 83 | 63.4 | ||
Mother | 124 | 94.7 | Stoma revision | ||
Education of thecare taker | Yes | 10 | 7.6 | ||
Primary | 68 | 51.9 | Stoma complications | ||
Secondary | 53 | 40.5 | Dermatitis | 54 | 41.1 |
Tertiary | 10 | 7.6 | Prolapse | 5 | 3.8 |
Monthly income | SAM | 2 | 1.5 | ||
0-500,000/=UGX | 106 | 80.9 | Retraction | 3 | 2.3 |
>500,000/=UGX | 25 | 19.1 | >1 complication | 19 | 14.5 |
Stoma indication | Stenosis | 4 |
| ||
Anorectal malformation | 77 | 58.8 | I.O | 2 |
|
Hirschsprungs disease | 25 | 19.1 | Presence--of—stoma complications | ||
Intussusception | 19 | 14.5 | Yes | 83 | 63.4 |
Intestinal obstruction or perforation | 10 | 7.6 | No | 48 | 36.6 |
Age at stomaplacement | Stoma duration | ||||
0-1 month | 67 | 51.2 | 1-6months | 45 | 34.4 |
1-12 months | 46 | 35.1 | 6-12months | 40 | 30.5 |
>12 | 18 | 13.8 | 12-36months | 42 | 31.3 |
>36months | 5 | 3.8 | |||
Table 1: Participant characteristics.
The mean age at the time of stoma placement was 1 and a half years (SD±0.7month). The most common indication for intestinal stomas was Anorectal malformations followed by Hirschsprungs disease and intussusception with 77 (58.8%), 25 (19.1%) and 19 (14.5%) patients respectively. Sixty five percent of the stomas were placed by residents and the most exteriorised part was sigmoid colon 104 (79.4%). Majority of children had intestinal stomas for more than 6 months 86 (65.6%) and all stomas were temporary.
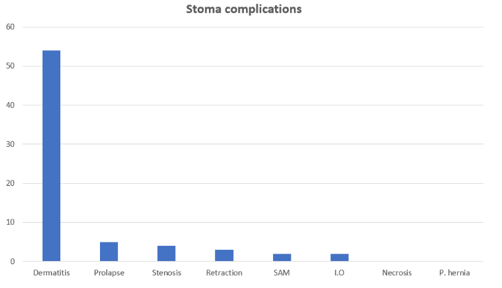
The prevalence of intestinal stoma complications among children in our setting was 63.4 % (83/131) with the most common complication being dermatitis followed by stoma prolapse at 54 (41.1%) and 5 (3.8%) respectively as shown in figure 1. Other complications including stoma retraction, stenosis malnutrition and intestinal obstruction were significantly low ranging from 1.5-3% as shown in figure 1. Stoma revision was required in 10 (7.4%) of children especially with prolapse, stenosis, retraction and intestinal obstruction.
According to bivariate analysis, the following factors were significant; age at stoma placement 1-12months and above 12months (OR 2.8 and 4.9 with p-value =0.015 and p-value=0.02, respectively), caretakers of primary education (p-value=0.011), monthly income ≤500,000/=UGX (p-value=0.009), indication being an Intussusception (OR 4, p-value=0.039), Ileostomy (p-value=0.005) and stoma duration of 12 to <36 p-value=0.028 p-value=0.035)> Characteristic Chi square test Frequency (%) Bivariate analysis Multivariate analysis Presence—of complications p- value Crude-OR P-value Adjusted-OR (95% CI) p-value Yes No 0..007 34(50.8) 33(49.3) 67 (51.2) 1 1 34(73.9) 12(26.1) 46 (35.1) 2.8 0.015 2 (0.56-6.93) 0.292 15(83.3) 13(16.7) 18 (13.8) 4.9 0.02 10.7(1.47-17.62) 0.019 0.785 47(64.4) 26(35.6) 73 (55.7) 1 1 36(62.1) 22(37.9) 58 (44.3) 0.9 0.785 1(0.37-2.93) 0.939 0.801 45(64.3) 25(35.7) 70 (53.4) 1 11(68.8) 5(31.3) 16 (12.2) 1.2 0.736 0.9 (0.23-3.75) 0.909 27(60.0) 18(40.0) 45 (34.4) 0.8 0.643 0.7(0.24-1.89) 0.454 0.247 80(64.5) 44(35.5) 124 (94.7) 1 1 3(42.9) 4(57.1) 7 (5.3) 0.4 0.26 0.37(0.05-2.77) 0.333 0.037 50(73.5) 18(26.5) 68 (51.9) 1 1 27(50.9) 26(49.1) 53 (40.5) 0.4 0.011 0.4(0.15-1.1) 0.077 6(60) 4(40) 10 (7.6) 0.5 0.38 0.9(0.16-5.6) 0.946 0.007 73(68.9) 33(31.1) 106 (80.9) 1 1 10(40) 15(60) 25 (19.1) 0.3 0.009 0.5 (0.15-1.61) 0.246 0.169 44(57.1) 33(42.9) 77 (58.8) 1 1 16(64) 9(36) 25 (19.1) 1.3 0.546 1.06(0.28-4) 0.934 16(84.2) 3(15.8) 19 (14.5) 4 0.039 0.03(0-1.26) 0.066 7(70) 3(30) 10 (7.6) 1.8 0.442 0.08(0-2.36) 0.142 0.002 24(88.9) 3(11.1) 27 (20.6) 1 1 59(56.7) 45(43.3) 104 (79.4) 0.2 0.005 0.02 (0-0.66) 0.028 0.825 31(64.6) 17(35.4) 48 (36.6) 1 52(62.7) 31(37.4) 83 (63.4) 0.9 0.825 0.894 54(62.8) 32(37.2) 86 (65.7) 1 25(65.8) 13(34.2) 38 (29) 1.1 0.749 0.6(0.19-1.73) 0.327 4(57.1) 3(42.9) 7 (5.3) 0.8 0.767 0.3(0.02-5.05) 0.44 0.103 35(77.8) 10(22.2) 45 (34.4) 1 22(55) 18(45) 40 (30.5) 0.3 0.028 0.3 (0.1-1.16) 0.085 23(56.1) 18(43.9) 42 (31.3) 0.4 0.035 0.4(0.11-1.16) 0.088 3(60) 2(40) 5 (3.8) 0.4 0.388 0.5(0.05-5) 0.542 0.278 81(62.8) 48(37.2) 2(100) 0(0) Age at stoma placement 0-1 month 1-12 months >12 Sex Male Female Residence Nearby Surrounding districts Far districts Attendant relationship Mother Others Education of the care taker Primary Secondary Tertiary Monthly income 0-500,000/=UGX >500,000/=UGX Stoma indication Anorectal malformation Hirschsprungs disease Intussusception Intestinal obstruction orperforation Exteriorised part Ileostomy Colostomy Theatre used Casualty Main Cadre of the surgeon Resident Fellow Surgeon Stoma duration 1-6months 6-12months 12-36months >36months Type of stoma Divided End
Table 2: Analysis of the factors associated with intestinal stoma complication
According to multivariate analysis, the significant factors were age at stoma placement of above 12 months (OR 10.7, CI 1.47-17.62, p-value=0.019) and exteriorization of the ileum (CI 0-0.66, p-value=0.028) as shown in table 2.
Discussion
Intestinal stomas are an important integral part in the management of children with gastrointestinal disorders hence many children live with these stomas as well as associated complications.
We found male children to have more intestinal stomas than female children with a male to female ratio of 1.3:1. This is comparable to findings from other studies including in Aba Nigeria where a male to female ratio of 2:1 was found, in Benin city Nigeria where a male to female ratio of 2.8:1 was found and 1.7:1 in India [1,8,9]. The higher prevalence of intestinal stomas among males is probably because the commonest indications are intussusception and ARM which commonly occur in males.
The most common indications for intestinal stomas were congenital anomalies among which ARMs were the commonest followed by HD. This is similar to findings from other studies [1,3,4]. All our patients had temporary intestinal stomas because they had correctable lesions.
In our study we found a high prevalence of intestinal stoma complications of 63.4%which is comparable to the worldwide complication rate reported in other literature of 28-74% [7]. This is however higher than in Nigeria where a complication rate of 33% was found [9] and in India where a rate of 45% was found [8] and lower than in Tanzania where a complication rate of 81.4% was found by Massenga and colleagues [3]. The differences in complication rates are due to the differences in the recruited age groups for example in Tanzania, children up to 18 years were recruited whereas in our study only children up to 12 years were recruited. Also, the methods of assessing for complications differ in different places with no standardized definition for the individual complications which causes variability in the reported rates. The differences in economic status and education levels amongst patients in these studies also explains why differing rates are reported as poor caretakers with Uneducation have been reported to have more children with complications than the rest.
The peristomal dermatitis rate of 41.1% found in our children is lower than that found in Nigeria of 84.8% in Benin city [1] and 70% in Aba state [9]. The higher rates of dermatitis in these states were reported to be because of the poor care of intestinal stomas amongst their patients as most of them were uneducated and from poor and remote families. Similar problems are faced by our patients but probably with better stoma care. This is in contrary to studies elsewhere where lower rates of dermatitis have been reported for example 20% in India [8] and 7% in Tanzania [3]. The lower rates in these studies may be due to the difference in the populations studied as these also included adult patients.
Peristomal dermatitis is mainly a problem of ileostomies and in this study, we found 88.9% of patients with ileostomies having complications in comparison with 56.7% of patients with colostomies. This is comparable to findings by Shellito and colleagues of 70-84.6
Limitations
The Cross-sectional nature of the study limits causal inference and hospital records might have limited data quality. Data from this study is limited to the current complications the child had at the time of the study therefore, we might have missed complications that happened before the study and were no longer present at the time of the study. Non-probability sampling method was used hence we cannot rule out selection bias.
Conclusion
Intestinal stoma complications in children are high in our setting with peristomal dermatitis being the most common complication followed by stoma prolapse. Stomas placed in children aged above 12 months and exteriorization of the ileum are associated with an increased risk of getting stoma complications at 10.7 times and 80% respectively. We recommend that children with ileostomies be prioritized for stoma reversals to minimize development of complications but also to reduce the period with which they have to live with the stoma and its complications. Sigmoid divided colostomies where indicated should be used in all children as these are associated with the fewest complications rates. Patients with ileostomies and stomas placed after one year of life should have regular periodic scheduled appointments for review so that complications are diagnosed early and managed appropriately. A further analysis of the factors associated with peristomal dermatitis in children including use of barrier creams, adequacy of information on stoma care and access to stoma supplies may help in alleviating this common complication. Another study that describes the complications following intestinal stoma reversals in children can be carried out to further document this burden and devise preventive measures.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Od O, Eo O, Ec O, Osifo O D. (2008). Colostomy in Children: Indications and Common Problems in Benin City, Nigeria. Pak J Med Sci. 24: 199–203.
View at Publisher | View at Google Scholar - Çiğdem MK, Onen A, Duran H, Öztürk H, Otçu S. (2006). The mechanical complications of colostomy in infants and children: analysis of 473 cases of a single center. Pediatric Surgery International. 22:8 22: 671–676.
View at Publisher | View at Google Scholar - Massenga A, Chibwae A, Nuri AA, Bugimbi M, Munisi YK, et al. (2019). Indications for and complications of intestinal stomas in the children and adults at a tertiary care hospital in a resource-limited setting: A Tanzanian experience. BMC Gastroenterol. 19.
View at Publisher | View at Google Scholar - Muzira A, Kakembo N, Kisa P, Langer M, Sekabira J, et al. (2018). The socioeconomic impact of a pediatric ostomy in Uganda: a pilot study. Pediatr Surg Int. 34: 457–466.
View at Publisher | View at Google Scholar - Ahmad Z, Sharma A, Saxena P, Choudhary A, Ahmed M. (2013). A clinical study of intestinal stomas: its indications and complications. Int J Res Med Sci. 1: 536.
View at Publisher | View at Google Scholar - Cottam J, Richards K, Hasted A, Blackman A. (2007). Results of a nationwide prospective audit of stoma complications within 3 weeks of surgery. Colorectal Dis. 9: 834–838.
View at Publisher | View at Google Scholar - Vriesman MH, Noor N, Koppen IJ, di Lorenzo C, de Jong JR, et al. (2020). Outcomes after enterostomies in children with and without motility disorders: A description and comparison of postoperative complications. J Pediatr Surg. 55.
View at Publisher | View at Google Scholar - Chanchlani R, Shrivastava D. (2019). Indications and complications of colostomy in newborn: our experience. International Surgery Journal. 7.
View at Publisher | View at Google Scholar - Samuel Chidi E. (2018). Childhood Colostomy and Its Complications in Aba, Nigeria. International Journal of Clinical and Experimental Medical Sciences. 4: 32.
View at Publisher | View at Google Scholar - Lau JTK. (1983). Proximal end transverse colostomy in children - A method to avoid colostomy prolapse in Hirschsprung’s disease. Dis Colon Rectum. 26: 221–222.
View at Publisher | View at Google Scholar - Lokale HJ. (2019). Health Related Quality of Life of Children with Intestinal stomas, a cross-sectional study at Mulago Hospital.
View at Publisher | View at Google Scholar - Park JJ, del Pino A, Orsay CP, Nelson RL, Pearl RK, et al. (1999). Stoma complications: The Cook County Hospital experience. Dis Colon Rectum. 42: 1575–1580.
View at Publisher | View at Google Scholar - Cheung MT. (1995). Complications of An Abdominal Stoma: An Analysis Of 322 Stomas. Z J Surg. 65: 808–881.
View at Publisher | View at Google Scholar - Shabbir J, Britton DC. (2010). Stoma complications: a literature overview. Colorectal disease: the official journal of the Association of Coloproctology of Great Britain and Ireland. pp. 958–964.
View at Publisher | View at Google Scholar - Shellito PC. (1998). Complications of abdominal stoma surgery. Dis Colon Rectum. 41: 1562–1572.
View at Publisher | View at Google Scholar - Hellman J, Lago CP. (1990). Dermatologic complications in colostomy and ileostomy patients. Int J Dermatol. 29: 129–133.
View at Publisher | View at Google Scholar - Kargl S, Wagner O, Pumberger W. (2016). Ileostomy Complications in Infants less than 1500 grams – Frequent but Manageable. J Neonatal Surg. 6.
View at Publisher | View at Google Scholar - Stensrud KJ, Emblem R, Bjørnland K. (2012). Late diagnosis of Hirschsprung disease-patient characteristics and results. J Pediatr Surg. 47: 1874–1879.
View at Publisher | View at Google Scholar - McCready RA, Beart RW. (1980). Adult Hirschsprung’s disease: Results of surgical treatment at mayo clinic. Dis Colon Rectum. 23: 401–407.
View at Publisher | View at Google Scholar - Shah M, Napar NB, Jhammat FI, Arshad HS, Saleem M. (2020). Comparison of frequency of complications in loop versus divided colostomy in patients with high variety anorectal malformation. J Neonatal Surg. 9.
View at Publisher | View at Google Scholar - Mahjoubi B, Moghimi A, Mirzaei R, Bijari A. (2005). Evaluation of the end colostomy complications and the risk factors influencing them in Iranian patients. Colorectal Disease. 7: 582–587.
View at Publisher | View at Google Scholar

 Clinic
Clinic
