Case report | DOI: https://doi.org/10.31579/2834-796X/067
Popliteal artery aneurysm treated with endovascular technique and new device: case report and literature review
- Rafael de Athayde Soares *
- Marcus Vinícius Martins Cury
- Aline Yoshimi Futigami
Rafael de Athayde Soares, Hospital do Servidor Público Estadual de São Paulo, Iamspe.
*Corresponding Author: Rafael de Athayde Soares, Hospital do Servidor Público Estadual de São Paulo, Iamspe.
Citation: Rafael de A. Soares, Marcus V. Martins Cury and Aline Y. Futigami, (2024), Popliteal artery aneurysm treated with endovascular technique and new device: case report and literature review, International Journal of Cardiovascular Medicine, 3(3); DOI:10.31579/2834-796X/067
Copyright: © 2024, Rafael de Athayde Soares. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 07 June 2024 | Accepted: 21 June 2024 | Published: 28 June 2024
Keywords: popliteal artery; endovascular surgery; popliteal artery aneurysm
Abstract
In this paper, we aimed to report an alternative endovascular treatment in a patient with an isolated popliteal artery aneurysm. A 69 year-old male patient, with hypertension and post-operative of gastric bypass surgery for obesity, was admitted with right limb pain, mainly in the calf, associated with a weakness and difficulty walking. The patient was submitted to a duplex ultrasound, that suggested a popliteal artery aneurysm, with 3,8 cm diameter, confirmed with CT angiogram. Furthermore, the patient had no proper saphenous vein diameter for a open surgery bypass evaluated by a Doppler ultrasound. Then, the patient was scheduled to undergo endovascular treatment of the popliteal artery aneurysm with two covered self-expandable 8x100 and 10x75 Merit Wrapsodyâ. The patient was discharged from the hospital two days after the surgery with no complications, palpable pedal pulses taking Rivaroxaban 20mg and Clopidogrel 75mg daily. At year follow-up the patient was asymptomatic and duplex showed patent stent without evidence of endoleak.
Introduction
It is well known in literature that popliteal artery aneurysm represents 70% of all peripheral arterial aneurysm (PAA), furthermore the most common surgical treatment is ligation of the popliteal aneurysms associated with a femoro-popliteal bypass with the great saphenous vein.1 PAA prevalence is estimated to be 1% in men aged 60–80 years, affecting women less frequently, with a male to female ratio of 20:1.2
Untreated PAA natural course includes a high incidence of acute and thromboembolic complications, with 50% of patients presenting with such symptoms as intermittent claudication, rest pain, blue toe syndrome, or acral necrosis.2 Approximately 30% of untreated patients with PAA experience acute thrombosis and distal embolization, with amputation rates of up to 20%.3,4,5 The gold standard for PAA treatment consists of open surgery with with limb salvage rates of 86–99% and primary patency rates of 66–86% over 5 years.3 However in high cardiac risk patients and patients with no proper autologous vein substitute the endovascular treatment for PAA has been proved as a safety and effective therapy. Previous studies assumed that endovascular therapy provides similar results to open surgery for PAA.6,7
In this study, we describe an option for endovascular treatment in a patient with an isolated popliteal aneurysm with a new device. The Research Ethics Committee approved this study (decision number 32380920.5.0000.5464).
Case Report
A 69 year-old male patient, with hypertension and post-operative of gastric bypass surgery for obesity, was admitted with right limb pain, mainly in the calf, associated with a weakness and difficulty walking, likewise a claudication symptom. On physical examination, he had a good general health, with a pulsating bulge with fibroelastic consistency palpable in the right popliteal region. The patient had femoral, popliteal and distal pulses present bilaterally. The patient was submitted to a duplex ultrasound, that suggested a popliteal artery aneurysm, with 3,8 cm diameter with thrombi and then was submitted to a computed tomography angiography (CTA) of the abdomen, pelvis and inferior limbs bilaterally. The CTA showed no other abnormalities in the arterial system, except for an isolated right popliteal artery aneurysm, with 3,8 cm diameter and thrombi associated. (Figure 1). The distance between the end of the popliteal artery aneurysm and the knee joint interline was 1,1cm. The proximal landing zone had 8,4mm diameter and distal landing zone had 6,7mm diameter. The total length of the PAA was 7,67cm. The patient was submitted to a duplex ultrasound in order to evaluate the great saphenous vein diameter, and it was inadequate for a open bypass, due to diameter < 3mm>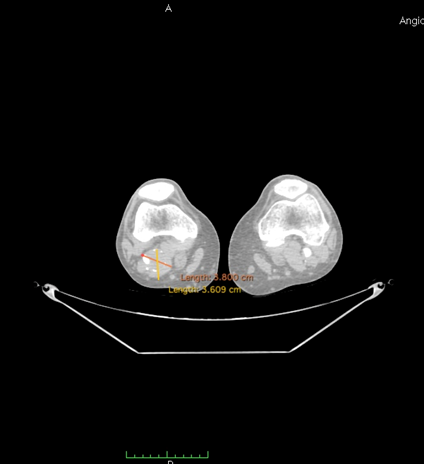
Figure 1: Angio-CT scan in axial incidence showing popliteal artery aneurysm (PPA).
The patient was scheduled to undergo endovascular treatment of the popliteal artery aneurysm. Under general anesthesia, a right common femoral artery was antegrade punctured guided with a duplex ultrasound to perform the whole intervention percutaneously with a 6F 11cm sheat. After the puncture, the Perclose Proglideâ was inserted, in order to preload and guarantee the sealing of the puncture. Then, a 0,035”260cm Terumo â was used to perform the crossing over the distal arteries. The patient was heparinized with 5000UI intravenous in bolus. We performed a right limb arteriography to confirm the popliteal artery aneurysm (Figure 2). The popliteal artery was properly catheterized and we changed the guidewire for an Amplatz 0,035”260cm, in order to place a 11cm 11F sheat. After proper evaluation, two a covered self-expandable 8x100 and 10x75 Merit Wrapsodyâ were placed under roadmap into the distal popliteal artery and proximal femoral artery respectively, and post dilatated with a 8x100 and 10x100 catheter balloon Oceanus figures 3 and 4. There were no endoleaks, and the popliteal artery patency was identified. All the materials were removed, and we completed the final step of the perclose Proglideâ puncture closing. The patient was transferred to the nursery room, being discharged from the hospital two days after the surgery with no complications, femoral, popliteal and podal pulses present bilaterally, taking Rivaroxaban 20mg / day and Clopidogrel 75mg/day. After 1 month the patient was evaluated, presenting no further symptoms, no palpable mass in the right popliteal artery, and was submitted to a Duplex Ultrasound (Figure 5), that showed deep popliteal artery patency, stent patency, reduction of the aneurysm sac and no endoleaks. Furthermore, after one year follow-up, the patient remained asymptomatic, with Duplex Ultrasound showing popliteal artery with stent patency and no endoleaks. (Figure 6).
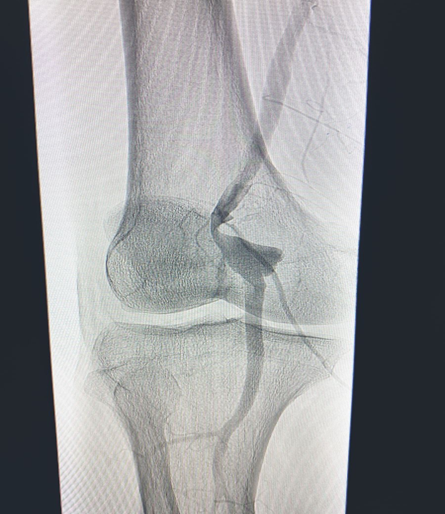
Figure 2: Arteriography showing PPA.
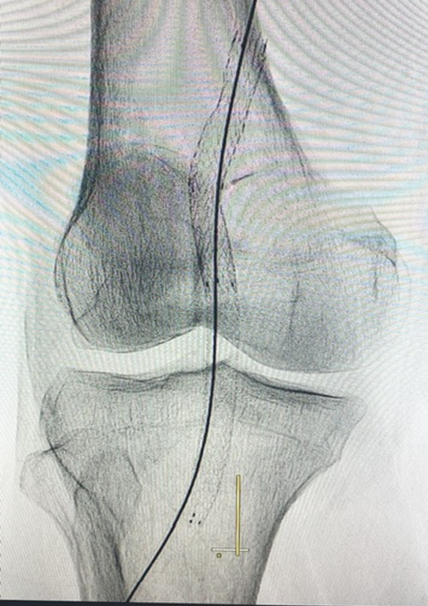
Figure 3: Post-operative arteriography showing covered self-expandable 8x100 and 10x75 Wrapsodyâ into the popliteal artery.
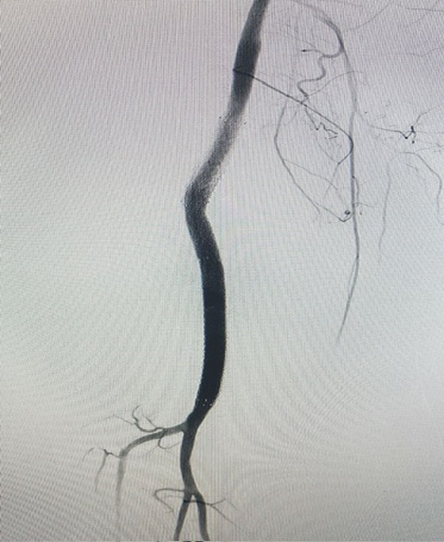
Figure 4: Post-operative arteriography showing covered self-expandable 8x100 and 10x75 Wrapsodyâ into the popliteal artery.
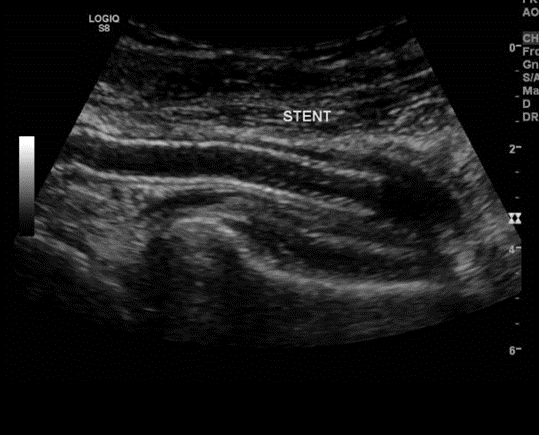
Figure 5: Duplex Ultrasound showing popliteal artery patency, stent patency and no endoleaks at 1 month.

Figure 6: Duplex Ultrasound showing popliteal artery patency, stent patency and no endoleaks at 1 year.
Discussion
Currently, high quality studies comparing the main repair methods of PAA are lacking. All currently published data on endovascular repair for PAA come from a heterogeneous patient population. Popliteal artery aneurysms (PAAs) represent 70% of peripheral aneurysms. Despite this, their estimated incidence is <0>65 years and have two characteristic features: they are often bilateral, and in 40% to 60% of cases, aneurysmal disease is also observed at other levels. Most PAAs are asymptomatic, although up to 30% may show complications, especially those related to embolization to infrapopliteal vessels or aneurysm thrombosis. PAA rupture has only rarely been reported.8
Nowadays, the two most widely accepted therapeutic options for the treatment of a PAA are exclusion, followed by venous or prosthetic bypass and the use of a stent graft for endovascular repair. In a prospective randomized trial comparing the open repair and endovascular treatment of asymptomatic PAAs, 15 PAAs were treated using the Viabahn stent graft, and a further 15 were surgically treated. Mean follow-up was 46 months.9 Results revealed no significant differences between the two groups: primary patency at 12 months was 100% for the open repair group and 87% for the endovascular repair group. Furthermore in another paper,10 these same authors reported similar midterm results for 27 patients in their open surgery
group and 21 in the endovascular treatment group, including no difference in 6-year patency.
In this present paper we describe a patient that was not suitable for open surgery repair, since the duplex ultrasound demonstrated an inadequate great saphenous vein diameter for proper bypass. As an option, the endovascular repair was conducted for the patient. Joshi et al11 performed a metanalysis regarding endovascular and open surgery treatment for PAA where they found that at one year there is moderate‐certainty evidence that primary patency may be improved in the surgery group but assisted primary patency rates were similar between groups. At four years there was no clear benefit from either endovascular stent graft or surgery to primary or assisted primary patency (moderate‐certainty evidence). As both operating time and hospital stay were reduced in the endovascular group (moderate‐certainty evidence), it may represent a viable alternative to open repair of PAA.
The advantages of endovascular repair are low invasiveness, minor blood loss; and a short duration of intervention. Further major benefits of this minimally invasive procedure are a short hospitalization and short recovery times with fewer wound complications. However, the use of endovascular repair is limited by the patient's anatomy. For a successful stent graft implantation, patients with at least two runoff vessels and suitable proximal and distal landing zones (2 cm) are preferred.12 However, graft thrombosis is more likely following endovascular repair during the first 30 post-operative days. Reasons for early stent graft thrombosis include inadequate stent graft expansion, stent graft kinking, or inappropriate inhibition of platelet aggregation.13 Therefore, the stent graft material, which is placed into the popliteal artery, needs to be very flexible. The popliteal artery is bent many times daily, which is associated with popliteal artery compression or occlusion. Due to this anatomical condition, common complications of endovascular repair for PAA are stent graft thrombosis, migration, kinking, fractures, and the occurrence of endoleaks.12,13
Merit Wrapsodyâ are flexible self-expanding endoprosthesis indicated for use in hemodialysis patients for the treatment of stenosis or occlusion within the dialysis outflow circuit of an arteriovenous (AV) fistula or AV graft, consisted of Nitinol, ePTFE, PTFE structure. Several papers showed encouraging results regarding the target lesion primary patency at 30 days of 100% (45 of 45 patients had reached 30 days of follow-up). The target lesion primary patency for the patients who had completed 12 months of follow-up was 84.6% (33 of 39).14 Due to the flexibility of the Merit Wrapsodyâ it may be considered a feasible endograft for using in popliteal aneurysms. There was a lack at Viabahn stent graft commercialization in Brazil in the period where this patient was submitted to PAA correction, leading to a necessity for using another stent graft for endovascular repair.
This case report has some limitations, since it is a single case report, with no long-term follow-up. Larger studies should be performed in order to evaluate the safety and efficacy of endovascular treatment with Merit Wrapsodyâ for PAA.
Conclusion
Endovascular treatment with Merit Wrapsodyâ
covered stents for PAA seens to be a safety and effective alternative for treating minimally invasive this condition, leading to an adequate flow sealing and proper aneurysm exclusion. Further and more robust studies are needed to validate this preliminary results.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The Authors declare that there is no conflict of interest regarding this paper.
Informed consent has been obtained from the patient for publication of the case report and accompanying images.
References
- Cecenarro RR, Allende JN, Barreras Molinelli L, et al. (2018). Popliteal artery aneurysms: Literature review and presentation of case. Rev Fac Cien Med Univ Nac Cordoba. 75(1):41–45.
View at Publisher | View at Google Scholar - Rutherford R.B. (2005). Arterial aneurysms. in: Cronenwett J.L. Rutherford's vascular surgery. 6th ed. Saunders, Philadelphia, PA 1403-1408.
View at Publisher | View at Google Scholar - Kropman R.H, De Vries J.P, Moll F.L. (2007). Surgical and endovascular treatment of atherosclerotic popliteal artery aneurysms. J Cardiovasc Surg (Torino). 48: 281-288.
View at Publisher | View at Google Scholar - Dawson I, Sie R.B, van Bockel J.H. (1997). Atherosclerotic popliteal aneurysm. Br J Surg. 84: 293-299.
View at Publisher | View at Google Scholar - Kropman R.H, Schrijver A.M, Kelder J.C, Moll F.L, de Vries J.P. (2010). Clinical outcome of acute leg ischaemia due to thrombosed popliteal artery aneurysm: systematic review of 895 cases. Eur J Vasc Endovasc Surg. 39: 452-457.
View at Publisher | View at Google Scholar - Tielliu I.F, Verhoeven E.L, Zeebregts C.J, Prins T.R, Bos W.T, Van den Dungen J.J. (2007). Endovascular treatment of popliteal artery aneurysms: is the technique a valid alternative to open surgery?. J Cardiovasc Surg (Torino). 48: 275-279.
View at Publisher | View at Google Scholar - Saunders J.H, Abisi S, Altaf N, Yong Y, MacSweeney S.T, Whittaker S. et al. (2014). Long-term outcome of endovascular repair of popliteal artery aneurysm present a credible alternative to open surgery. Cardiovasc Intervent Radiol. 37: 914-919.
View at Publisher | View at Google Scholar - Galland R.B. (2008). History of the management of popliteal artery aneurysms. Eur J Vasc Endovasc Surg. 35: 466-472.
View at Publisher | View at Google Scholar - Antonello M, Frigatti P, Battocchio P, Lepidi S, Cognolato D, Dall’Antonia A. et al. (2005). Open repair versus endovascular treatment for asymptomatic popliteal artery aneurysm: results of a prospective randomized study. J Vasc Surg. 42: 185-193.
View at Publisher | View at Google Scholar - Antonello M, Frigatti P, Battocchio P, Lepidi S, Dall’Antonia A, Deriu G.P. et al. (2007). Endovascular treatment for asymptomatic popliteal artery aneurysm: 8-year concurrent comparison with open repair. J Cardiovasc Surg (Torino). 48: 267-274.
View at Publisher | View at Google Scholar - Joshi D., James R.L., Jones L. (2014). Endovascular versus open repair of asymptomatic popliteal artery aneurysm. Cochrane Database Syst Rev. 8: CD010149.
View at Publisher | View at Google Scholar - Siauw R, Koh E.H, Walker S.R. (2006). Endovascular repair of popliteal artery aneurysms: techniques, current evidence and recent experience. ANZ J Surg. 76: 505-511.
View at Publisher | View at Google Scholar - Cook S, Windecker S. (2009). Early stent thrombosis: past, present, and future. Circulation. 119: 657-659.
View at Publisher | View at Google Scholar - Gilbert J. Prospective First-in-Human Study of the Merit WRAPSODY Endovascular Stent Graft for Treatment of Access Circuit Outflow Stenosis in Hemodialysis Patients. Journal of Vascular Surgery Abstracts 7S Volume 75, Number 4S.
View at Publisher | View at Google Scholar

 Clinic
Clinic
