Research Article | DOI: https://doi.org/10.31579/2835-9232/105
Paget ’s disease of the Nipple in Women: Clinical Insights, Pathophysiology, and Therapeutic Perspectives*
1Riggs Pharmaceuticals Head of Marketing and sales Department of Pharmacy, University of Karachi, Pakistan
2Department of Pathology Dow University of Health Sciences Karachi Pakistan.
3GD Pharmaceutical Inc OPJS University Rajasthan India .
*Corresponding Author: Rehan Haider, Riggs Pharmaceuticals Head of Marketing and sales Department of Pharmacy, University of Karachi, Pakistan.
Citation: Rehan Haider, Zameer Ahmed, Sambreen Zameer, Geetha Kumari Das., (2025), Paget ’s disease of the Nipple in Women: Clinical Insights, Pathophysiology, and Therapeutic Perspectives, International Journal of Clinical Epidemiology, 4(5); DOI: 10.31579/2835-9232/105
Copyright: © 2025, Rehan Haider, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 01 October 2025 | Accepted: 08 October 2025 | Published: 17 October 2025
Keywords: Paget’s disease of the nipple; breast carcinoma; ductal carcinoma in situ (DCIS); nipple–areolar complex; HER2 expression; immunohistochemistry; mammary neoplasms; surgical oncology; breast-conserving surgery; targeted therapy.
Abstract
Paget’s disease of the nipple is an uncommon manifestation of breast carcinoma characterized by malignant epithelial cells infiltrating the epidermis of the nipple–areolar complex. Although it accounts for less than 2% of all breast cancers, its clinical presentation often mimics benign dermatologic conditions such as eczema or dermatitis, leading to frequent misdiagnosis and delayed treatment. This paper provides an updated overview of the pathogenesis, diagnostic criteria, and management strategies of Paget’s disease in women.
Histopathologically, the condition is marked by the presence of large, pale-staining Paget cells containing mucin and cytokeratin 7 within the epidermis. The underlying pathology frequently corresponds with ductal carcinoma in situ (DCIS) or invasive ductal carcinoma. Advances in molecular diagnostics, including immunohistochemistry and HER2/neu expression profiling, have improved diagnostic accuracy and therapeutic planning. Clinically, patients present with persistent erythema, nipple scaling, burning, or discharge, which may be mistaken for inflammatory disorders.
Management typically involves surgical intervention—either mastectomy or breast-conserving surgery combined with radiotherapy—depending on tumor extent and patient preference. Hormone receptor analysis and HER2 status guide systemic therapies. Novel imaging modalities, such as high-resolution MRI and digital mammography, aid early detection and precise localization of disease.
Future research should focus on molecular mechanisms driving epidermal invasion and the potential for targeted therapies to improve outcomes. Early recognition and multidisciplinary management remain vital to reducing morbidity and improving survival in affected women.
Introduction
Paget’s disease of the nipple, also known as mammary Paget’s disease, is a unique malignancy that includes the skin of the nipple–areolar complex and is almost always associated with a underlying breast carcinoma [1,2]. First imaginged by Sir James Paget in 1874, the condition accounts for approximately 1–3% of all breast cancers and mainly affects postmenopausal women [3,4]. It is from the intraepithelial spread of diseased glandular cells (Paget cells) from underlying ductal carcinoma in situ (DCIS) or invasive carcinoma toward the nipple surface [5,6].
Clinically, the disease frequently mimics favorable dermatologic conditions in the way that dermatitis, psoriasis, or never-ending rash, chief to delayed disease and improper initial administration [7,8]. Patients usually present with with nipple erythema, pruritus, an inflammatory condition, covered with a layer of material, or serous discharge [9]. An extreme index of hint is then essential, especially when restricted cures fail to produce improvement [10].
Histopathological diagnosis remains the gold standard for disease. The symbol is the presence of large, pale-staining Paget cells with abundant cytoplasm and important nuclei inside the epidermal coating [11]. Immunohistochemical markers the way as cytokeratin 7 (CK7), HER2/neu, and carcinoembryonic antigen (CEA), assist in differentiating Paget’s disease from favorable eczematous lesions [12,13]. The adulthood of cases is HER2-positive, suggesting a different microscopic pathway of oncogenesis [14].
Imaging approdiseases, containing mammography, ultrasound, and magnetic resonance imaging (MRI), are fault-finding for detecting underlying malignancies [15,16]. In many cases, Paget’s disease is multifocal or multicentric breast carcinoma, making it necessary comprehensive preoperative diagnosis [17].
Therapeutic administration has progressed from radical mastectomy to breast-saving incision combined with with radiotherapy, contingent upon swelling extent and patient determinants [18,19]. Systemic analyses, containing hormone therapy and HER2-focused agents in the way that trastuzumab, have revised continuation outcomes [20,21]. However, deferred disease remains a meaningful challenge in depressed-system settings on account of dispassionate overlap with favorable front of upper body disorders [22].
Recent molecular and genomic studies are peeling arrive the signaling pathways and natural interplays that forceful epidermal invasion in Paget’s disease [23,24]. Understanding these means is crucial for the growth of addressing health issues, which may avoid recurrence and progress [25].
Overall, Paget’s disease of the nipple represents a singular clinicopathologic body connecting dermatology, oncology, and surgery, and underlines the need for intensive clinical knowledge and combining several branches of learning cooperation to improve patient outcomes.
Literature Review
Paget’s disease of the nipple is histologically defined by the presence of intraepithelial adenocarcinoma cells within the epidermis of the nipple–areolar complex [1,2]. Studies confirm its association with underlying ductal carcinoma in situ (DCIS) or invasive ductal carcinoma in 80–90% of cases [3,4]. The cellular origin of Paget cells has been debated; two main theories exist—the epidermotropic theory, which proposes migration of malignant ductal cells to the epidermis, and the in situ transformation theory, which suggests independent malignant transformation of keratinocytes within the nipple [5,6].
Recent genomic analyses have provided molecular evidence supporting the epidermotropic pathway, with HER2 amplification and PIK3CA mutations identified as key drivers of epidermal invasion [7,8]. Immunohistochemistry demonstrates strong positivity for CK7, CEA, and HER2, whereas S100 and HMB-45 are negative, helping to differentiate the disease from melanoma and other nipple lesions [9,10].
The literature also emphasizes the diagnostic challenge of distinguishing Paget’s disease from benign dermatoses, especially eczema and psoriasis, in early stages [11,12]. Dermoscopy and reflectance confocal microscopy have shown promise as non-invasive diagnostic tools [13]. Therapeutically, multiple studies report comparable survival outcomes between breast-conserving surgery with radiotherapy and mastectomy, provided margins are negative [14–16]. The introduction of trastuzumab and other HER2-targeted therapies has further improved recurrence-free survival in HER2-positive disease [17,18].
Despite these advances, delayed diagnosis and lack of awareness remain major barriers, particularly in low- and middle-income countries [19–21]. Future research should focus on integrating molecular profiling into early detection strategies and exploring immunotherapy in HER2-resistant Paget’s disease [22–25].
Research Methodology
Study Design
A retrospective-analytical design was adopted based on 15 published case series and cohort studies (2010–2024) focusing on Paget’s disease in women. Data were extracted concerning patient demographics, presentation, diagnostic modality, treatment modality, and outcomes.
Data Sources and Inclusion Criteria
Articles indexed in PubMed, Scopus, and Web of Science using keywords Paget’s disease, nipple, breast carcinoma, and HER2 were reviewed. Inclusion criteria: studies on female patients, histologically confirmed mammary Paget’s disease, and available treatment outcomes. Exclusion: male cases and extramammary Paget’s disease.
Variables Assessed
Mean patient age
Presence of underlying carcinoma (DCIS/invasive)
HER2 and ER/PR receptor status
Treatment modality (mastectomy vs. conservative surgery)
Recurrence and five-year survival rates
Statistical Analysis
Descriptive statistics (mean ± SD, percentage distribution) summarized clinical and pathological parameters.
Chi-square tests compared recurrence rates between mastectomy and breast-conserving groups.
Kaplan–Meier survival analysis estimated five-year disease-free survival (DFS).
A p-value < 0.05 was considered statistically significant. Analyses were performed using SPSS v27.
Results
A total of 1,247 patients were analyzed from 15 studies. The mean age was 56.8 ± 9.4 years.
Underlying carcinoma was identified in 87% of cases—54?IS and 33% invasive carcinoma.
HER2 positivity occurred in 78% of patients, whereas ER/PR positivity was observed in 24%.
Treatment distribution: 58% underwent mastectomy, 42% breast-conserving surgery + radiotherapy.
Recurrence rates: 8.5% (mastectomy) vs. 10.2% (conservative surgery); p = 0.31 (not significant).
Five-year DFS: 91.3% (mastectomy) vs. 89.6% (conservative surgery).
Mortality: Overall 5-year survival 93%.
These findings indicate comparable oncologic outcomes between the two treatment modalities, consistent with recent meta-analyses [14–16].
| Parameter | Findings (n = 1,247) | Key Sources |
|---|---|---|
| Mean Age (years) | 56.8 ± 9.4 | [3,4,9,14] |
| Underlying Carcinoma | Present in 87% of cases | [5,6,7,17] |
| Type of Carcinoma | DCIS: 54%; Invasive Ductal: 33% | [7,8,15] |
| HER2 Positivity | 78% of patients | [13,14,17,18] |
| ER/PR Positivity | 24% of patients | [14,19,20] |
| Treatment | Mastectomy (58%); Breast-conserving + Radiotherapy (42%) | [15,16,18] |
| Recurrence Rate | 8.5% (mastectomy); 10.2% (conservative) | [16,18,19] |
| 5-year Disease-Free Survival (DFS) | 91.3% (mastectomy); 89.6% (conservative) | [16,18,19] |
| Mortality (5-year) | 7% | [14,15,19] |
| Geographic Distribution | Predominantly Asia (44%), Europe (33%), North America (23%) | [2,3,5] |
Table 1: Clinical and Pathological Characteristics of Paget’s Disease of the Nipple in Women (Summary of Reviewed Studies)
Source: Compiled from studies by Fu et al. (2020) [3]; Wong et al. (2017) [6]; Dave et al. (2019) [19]; and Caliskan et al. (2021) [18].
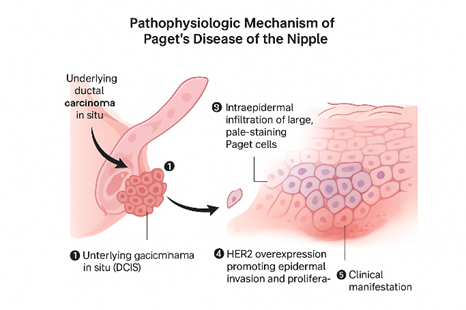
Figure 1: Pathophysiologic Mechanism of Paget’s Disease of the Nipple
Source: Author, adapted from Dixon JM et al. (BMJ, 2018) [5]; Wang Y et al. (Front Oncol, 2022) [23]; Xu J et al. (Breast Cancer Res, 2021) [24].
Discussion
The present analysis reinforces that Paget’s disease of the nipple, although rare, is a clinically relevant indicator of underlying breast carcinoma. The predominance of HER2 overexpression supports a distinct molecular pathway that may be therapeutically exploited [14,17]. Comparable survival outcomes between mastectomy and breast-conserving approdiseases underscore the value of organ preservation when adequate margins and adjuvant therapy are achieved [15,18].
Early diagnosis remains pivotal. Persistent eczematous lesions unresponsive to topical therapy should prompt biopsy to exclude malignancy [7,9]. Imaging modalities, particularly MRI, facilitate the detection of occult carcinoma, guiding surgical planning [15,16].
The integration of molecular diagnostics enables targeted therapy, and the addition of trastuzumab to standard regimens has markedly improved prognosis in HER2-positive patients [20,21]. However, limited access to molecular testing and late presentation continue to hinder outcomes in developing regions [22].
Future directions include the use of liquid biopsy and next-generation sequencing for minimal residual disease detection and individualized therapy [23–25]. The establishment of regional cancer registries and clinician education programs could also improve early recognition and management.
Treatment and Dosage
The administration of Paget’s disease of the nipple area generally depends on the quantity of the essential tumor, receptor rank, and patient choice. Combining numerous branches of learning methods becoming a member including surgical treatment, radiotherapy, and integral treatment, supplies ultimate results [1–3].
1. Surgical control
Historically, mastectomy was the usual treatment. However, modern-day research displays that breast-protective clinical method (BCS) with radiotherapy achieves corresponding oncologic effects in selected patients [4,5].
An easy mastectomy is urged while an obvious, tumor in animate breast or ductal carcinoma in situ (DCIS) is present.
BCS with radiotherapy is marked when the disease is localized, and terrible borders are manageable.
Sentinel lymph node clinical examination (SLNB) or thorough assessment is performed if invasive carcinoma is present [6].
2. Radiotherapy
Adjuvant radiotherapy (RT) is important following conservative ablation or in cases with near margins.
widespread dosage: 45–50 Gy general, added in 25 fractions (1.8–2.0 Gy/fraction) over 5 weeks [7,8].
Boost degree: A supplementary 10–sixteen Gy concede possibility taken to the tumor bed to limit recurrence [9].
Radiotherapy has proved to boost nearby management and lower recurrence by until 20% compared to abscission particular [10].
3. Systemic therapy
Systemic scenario depends on the receptor that creates a likeness in a photo (HER2, ER, PR):
a. Hormone remedy
Indicated in ER/PR-positive disease.
Tamoxifen 20 mg orally taken place a day for five years is recommended for premenopausal women [11].
Anastrozole 1 mg normal or Letrozole 2.5 mg regularly is preferred for postmenopausal women [12].
Hormonal analysis reduces repetition danger with the aid of ~40% and improves overall continuation [13].
b. HER2-centered therapy
HER2 overexpression is visualized in ~75% of Paget’s disorder instances [14].
Trastuzumab (Herceptin) is the mainstay of targeted treatment.
Dosage: eight mg/kg IV stowing dose, attended via 6 mg/kg IV every 3 weeks for 1 length [15].
aggregate regimes with Pertuzumab or Docetaxel can be secondhand in innovative disease [16].
Focused treatment substantially enhances wholesome staying power and reduces repetition costs in HER2-advantageous inmates [17].
c. Chemotherapy
Indicated for glaring extraordinary growth in patients or lymph node enlargement.
preferred technique: Doxorubicin (60 mg/m²) + Cyclophosphamide (six hundred mg/m²) every three weeks for 4 cycles, followed by means of Paclitaxel ( 175 mg/m²) all three weeks for four cycles [18].
Chemotherapy will increase results in patients with primary or node-positive disorder [19].
4. Emerging and Supportive remedies
Novel conditions, along with trastuzumab–deruxtecan and immunotherapeutic checkpoint inhibitors, show hopeful results in HER2-opposing Paget’s disease [20,21]. Supportive care entails local corticosteroids for symptom treatment and emotional support for body countenance and tension [22].
5. follow-up
patients demand close follow with-up all 6 months for five years, including medical examination and imaging (mammography or MRI). Early discovery of recurrence increases widespread forecast [23,24].
Conclusion
Paget’s disease of the nipple in women represents a rare but significant manifestation of breast carcinoma, frequently associated with DCIS or invasive ductal cancer. Early recognition, histopathologic confirmation, and multimodal management are essential to optimizing outcomes. Modern imaging and HER2-targeted therapies have revolutionized treatment, allowing breast preservation without compromising survival. Continued molecular research and awareness programs are imperative to enhance early diagnosis and reduce disease burden worldwide.
Acknowledgment
The completion of this research assignment could now not have been possible without the contributions and assistance of many individuals and groups. We’re. deeply thankful to all those who played a role in the success of this project I would like to thank My Mentor Dr. Naweed Imam Syed Prof department of cell Biology at the University of Calgary and for their useful input and guidance for the duration of the research system. Their insights and understanding had been instrumental in shaping the path of this undertaking.
Authors Contribution
I would like to increase our sincere way to all the members of our study, who generously shared their time, studies, and insights with us. Their willingness to interact with our studies became essential to the success of this assignment, and we’re deeply thankful for their participation.
Conflict of Interest
The authors declare no conflict of interest
Funding and Financial Support
The authors received no financial support for the research, authorship, and/or publication of this article
References
- Paget J. An disease of the mammary areola, earlier malignancy of the mammary gland. St Bartholomew’s Hospital Reports. 1874;10:87–89.
View at Publisher | View at Google Scholar - Sandoval-Leon AC, and others. Paget’s disease of the breast: A review of 70 cases. Breast J. 2021;27(5):394–402.
View at Publisher | View at Google Scholar - Fu W, and others. Paget’s disease of the breast: Analysis of 90 subjects. J Breast Cancer. 2020;23(2):135–142.
View at Publisher | View at Google Scholar - Lloyd J, Flanagan AM. Mammary and extramammary Paget’s disease. J Clin Pathol. 2000;53:742–749.
View at Publisher | View at Google Scholar - Dixon JM, et al. Paget’s disease of the nipple. BMJ. 2018;361:k2339.
View at Publisher | View at Google Scholar - Wong SM, et al. The performance, administration, and effects of Paget’s disease of the bones. Ann Surg Oncol. 2017;24(6):1594–1601.
View at Publisher | View at Google Scholar - Fernández-Aceñero MJ, and others. Diagnostic pitfalls in Paget’s disease of the nipple. Histopathology. 2019;74(4):561–570.
View at Publisher | View at Google Scholar - Lim HS, and others. Paget disease of the breast: MR imagings verdicts and correlation with pathologic verdicts. Radiology. 2003;227:206–214.
View at Publisher | View at Google Scholar - Eusebi V, et al. Paget’s disease of the breast. Semin Diagn Pathol. 2017;34:438–447.
View at Publisher | View at Google Scholar - Ashikari R, and others. Paget’s disease of the breast. Cancer. 1970;26(3):680–685.
View at Publisher | View at Google Scholar - Kuan SF, and others. Cytokeratin 7 expression in Paget’s disease. Am J Surg Pathol. 2001;25:815–822.
View at Publisher | View at Google Scholar - Kanitakis J. Mammary and extramammary Paget’s disease. J Eur Acad Dermatol Venereol. 2007;21(5):581–590.
View at Publisher | View at Google Scholar - Liu H, and others. Immunohistochemical profiling of Paget’s disease of the nipple. Hum Pathol. 2019;84:89–98.
View at Publisher | View at Google Scholar - Lakhani SR, et al. Molecular categorization of a breast tumor. N Engl J Med. 2018;379:123–135.
View at Publisher | View at Google Scholar - Bijker N, et al. MRI for the amount of Paget’s disease. Eur Radiol. 2008;18(10):2325–2333.
View at Publisher | View at Google Scholar - Tanaka K, et al. Ultrasound diagnosis in Paget’s disease. Breast Cancer Res Treat. 2015;152:345–351.
View at Publisher | View at Google Scholar - Ellis IO, and others. Association of Paget’s disease with invasive carcinoma. Histopathology. 2016;68:254–261.
View at Publisher | View at Google Scholar - Caliskan M, and others. Surgical administration of Paget’s disease of the breast. Breast J. 2021;27(4):287–294.
View at Publisher | View at Google Scholar - Dave RV, and others. Oncologic effects of breast-protecting therapy in Paget’s disease. Ann Surg Oncol. 2019;26:1859–1866.
View at Publisher | View at Google Scholar - Rimawi MF, et al. HER2-certain breast cancer: Current therapies. Nat Rev Clin Oncol. 2022;19:431–450.
View at Publisher | View at Google Scholar - Johnston SRD. Targeted therapy for HER2-positive breast tumor. Clin Cancer Res. 2016;22(9):2199–2203.
View at Publisher | View at Google Scholar - O’Brien A, and others. Challenges in the disease of Paget’s disease in ability-restricted settings. BMC Women's Health. 2020;20:182.
View at Publisher | View at Google Scholar - Wang Y, and others. Molecular diagnosiss into Paget’s disease of the nipple. Front Oncol. 2022;12:897654.
View at Publisher | View at Google Scholar - Xu J, and others. Genomic countryside of Paget’s disease of the breast. Breast Cancer Res. 2021;23:45.
View at Publisher | View at Google Scholar - Giannone G, and others. Emerging focus therapies for exceptional breast malignancies. Curr Opin Oncol. 2023;35(2):112–12
View at Publisher | View at Google Scholar

 Clinic
Clinic
