Research Article | DOI: https://doi.org/10.31579/2835-7957/111
Ketamine for the Critically Ill: Case Series and Clinical Reflections
- Ruchi Goyal *
- Lalit Gupta
Post Graduate Student Department of Anaesthesia and Critical Care Maulana Azad Medical College and Lok Nayak hospital, Bahadur Shah Zafar Marg, New Delhi-110002, India.
*Corresponding Author: Ruchi Goyal, Post Graduate Student Department of Anaesthesia and Critical Care Maulana Azad Medical College and Lok Nayak hospital, Bahadur Shah Zafar Marg, New Delhi-110002, India.
Citation: Ruchi Goyal, Lalit Gupta, (2024), Ketamine for the Critically Ill: Case Series and Clinical Reflections, Clinical Reviews and Case Reports, 4(3); DOI:10.31579/2835-7957/111
Copyright: © 2024, Ruchi Goyal. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 24 April 2025 | Accepted: 13 May 2025 | Published: 22 May 2025
Keywords: ketamine, critical care, ards, status asthmaticus, sedation, weaning, versatile, neuropathic pain
Abstract
Background: Considering its unique pharmacology, ketamine has become a subject of interest for various therapeutic applications in intensive care as a dissociative anesthetic agent. The primary objective of this case series is to demonstrate the importance of using ketamine among patients who are critically ill. Various critical presentations have been explored by utilizing ketamine as one of the management strategies for these patients. Methods: We report six cases from our ICU where ketamine was used as either an adjunct or primary modality of treatment. These include refractory status asthmaticus, ARDS, acute pain management in an opioid-tolerant patient, refractory delirium, acute agitation and anxiety in an intubated patient, and neuropathic pain management.
Results: In status asthmaticus, ketamine infusion improved bronchodilation and facilitated weaning from mechanical ventilation. In the course of ARDS, ketamine is allowed to reduce doses of sedatives and analgesics and to improve oxygenation. Ketamine provided effective analgesia in an opioid-tolerant patient and a patient with neuropathic pain. It also showed benefits in the management of refractory delirium, after which the level of consciousness and cooperation of the patient improved. Additionally, in a ventilated patient, intravenous ketamine lowered acute agitation and anxiety, followed by improved respiratory parameters.
Conclusions: This case series illustrates the diverse utility of ketamine in critical care, ranging from managing asthma, ARDS, acute pain, delirium, and agitation to neuropathy management. The unique properties of ketamine, specifically its bronchodilatory effects, analgesic properties, and probably neuroprotective effects, make it a beneficial pharmacological adjunct or primary treatment in many clinical scenarios. However, proper dosing titrations and careful selection of the patient, with monitoring for possible adverse effects, are crucial when using ketamine in critically ill patients. Further studies are needed on evidence-based parameters for the appropriate application of ketamine in the different scenarios occurring in critical care.
Introduction
Ketamine is a dissociative anesthetic agent that was first synthesized almost 60 years ago, similar in structure to phencyclidine. It is a Selective non-competitive N-Methyl-D-aspartate (NMDA) receptor antagonist prepared as a racemic mixture of two enantiomers, which have somewhat different affinities to receptors. Ketamine has gained increasing attention for its potential applications in critical care [1]. Historically, ketamine has been used for anesthesia and procedural sedation, but recently, a number of studies pointed out the peculiar properties that may benefit a large number of clinical scenarios seen in critically ill patients [2,3]. In this case series, we present six cases from our ICU where ketamine was used in an adjunct or primary treatment modality to exemplify this agent's versatility in diverse clinical scenarios.
Materials And Methods
Case 1: Refractory Status Asthmaticus
A 32-year-old female with a history of severe asthma was transferred to ICU from ward with refractory status asthmaticus. Her respiratory distress did not improve despite aggressive treatment with bronchodilators, corticosteroids and continuous nebulization with oxygen therapy. On discretion of ICU team, ketamine was initiated as a continuous infusion at a low dose of 0.1 mg/kg/hr and resulted in improved bronchodilation and a decrease in the work of breathing within 24 hours. The patient's condition stabilized, and she was successfully weaned off mechanical ventilation.
Case 2: Acute Respiratory Distress Syndrome (Ards)
A 56-year-old male patient developed severe ARDS as a complication to pneumonia and required deep sedation with paralysis for lung-protective ventilation in ICU. Ketamine was added to his sedation regimen at a dosage of 0.5 mg kg-1 h-1, after which other sedatives and analgesics were reduced. Oxygenation improved gradually over next 2-3 days, and there were no important adverse effects noted during the 10-day course of the ketamine infusion.
Case 3: Acute Pain Management In Opioid-Tolerant Patient
This 48-year-old male has a history of opioid dependence for his chronic lower back pain and was admitted to the ICU with septic shock after surgery for a perforated appendix on the 2nd day of surgery. His pain could not be controlled by conventional analgesic regimens along with opioids. Ketamine was initiated as an adjunct analgesic and used at a low dose of 0.1 mg/kg/hr, with improved pain control and reduction in opioid requirements without significant adverse effects. The patient was shifted to the surgical ward from the Intensive unit following a full recovery within 3 days.
Case 4: Refractory Delirium In A Critically Ill Patient
A 72-year-old female with severe sepsis developed refractory delirium despite optimal management with antipsychotics and environmental measures. Ketamine was added to her sedation regimen at a dose of 0.2 mg/kg/hr, leading to a significant improvement in her delirium symptoms within 24 hours. The patient's level of consciousness and cooperation improved, facilitating her participation in physical therapy and overall recovery.
Case 5: Acute Agitation And Anxiety In A Ventilated Patient
A 64-year-old male was in acute respiratory failure and required mechanical ventilation but became increasingly agitated and anxious, thereby compromising his ventilator management. A low-dose ketamine infusion of 0.1 mg/kg/hr was initiated, with significant abatement of agitation and improvement in respiratory parameters noted within hours. Gradually patient weaned off from the ventilator and shifted back to the medicine ward.
Case 6: Neuropathic Pain Management In A Critically Ill Patient
A 41-year-old female with Guillain-Barré syndrome was admitted to the ICU with very bad neuropathic pain refractory to conventional analgesics. After being started on the supplement of ketamine at a dosage of 0.3 mg/kg/hr, the patient showed dramatic pain relief and improved tolerance to physical therapy sessions without significant side effects. {table 1}
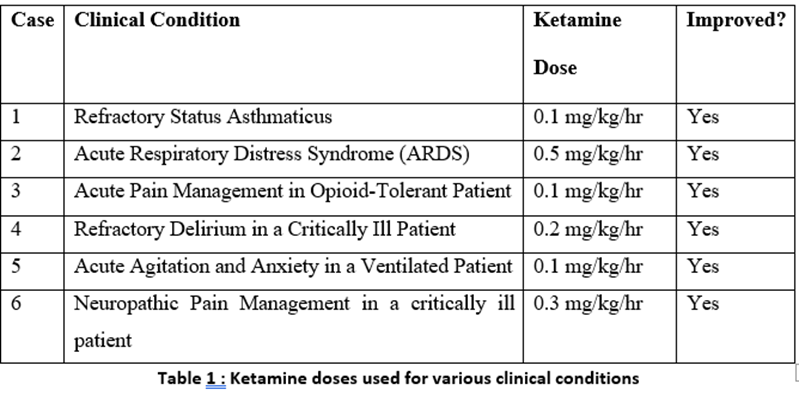
In our experience, ketamine demonstrated versatility in managing diverse clinical scenarios encountered in critically ill patients, including refractory asthma, ARDS, acute pain management, delirium, agitation, and neuropathic pain.
Results
In the case of refractory status asthmaticus, ketamine infusion resulted in improved bronchodilation and facilitated weaning from mechanical ventilation. In ARDS, ketamine allowed for a reduction in sedative and analgesic doses while improving oxygenation. Ketamine provided effective analgesia in an opioid-tolerant patient and a patient with neuropathic pain. It also demonstrated benefits in managing refractory delirium, improving the patient's level of consciousness and cooperation. Additionally, ketamine effectively reduced acute agitation and anxiety in a ventilated patient, leading to improved respiratory parameters.
Discussion
The cases presented in this series illustrate the diverse clinical indication and uses of ketamine in critical care. With the properties of bronchodilation, analgesia, and perhaps neuroprotective effects, it has been useful as an adjunct or even primary treatment for a range of life-threatening conditions in the critical care settingS. Stimulation of the N-methyl-D-aspartate receptor in the peripheral nervous system leads to release as norepinephrine and other catecholamines [1]. Common adverse effects of ketamine are due to this catecholamine release: tachycardia, hypertension, and bronchodilation [4]. This latter effect has led to use of ketamine as an adjunct therapy in status asthmaticus. In cases of refractory status asthmaticus and ARDS, the bronchodilatory effects of ketamine were harnessed to facilitate oxygenation and mechanical ventilation. This drug has been described to decrease airway resistance and increase compliance; thus, it may be a potential adjunct in the care of respiratory illnesses [5]. Ketamine has shown particular benefit in the management of acute pain in opioid-tolerant patients and neuropathic pain, as illustrated in Cases 3 and 6. The action mechanism of this compound uniquely involves antagonism at the NMDA receptor level, a very effective analgesia associated with low potential for respiratory depression normally associated with traditional opioid analgesics. Uprety et al. described the case report on the use of low-dose ketamine infusion as an adjuvant to opioids for pain management in a 31-year-old patient with sickle cell disease [6]. In this case report, a low-dose ketamine infusion was given to the patient, after which an improvement in subjective pain intensity and significant reduction in opioid dosage requirements were seen. These findings are in keeping with a prospective observational study that examined the use of ketamine in children presenting to the emergency department for status asthmaticus, with a loading dose of 1 mg/kg followed by an infusion of 0.75 mg/kg/h [7]. Ketamine reduced breathing frequency and clinical asthma score, comparable to the corresponding increase in oxygen saturations. Interestingly, ketamine has demonstrated potential benefits in the management of refractory delirium and agitation in critically ill patients, as illustrated in the cases 4 and 5. Delirium is a common and serious postoperative complication; some evidences suggest that intraoperative administration of subanaesthetic dose of ketamine for postoperative analgesia may have a role in preventing delirium [8,9]. Some critically ill patients on mechanical ventilation, often requiring continuous sedatives to quell agitation, reduce excessive oxygen consumption, and assist with care [10]. Nevertheless, prolonged sedation can lead to various negative outcomes such as extended stays in the intensive care unit (ICU), increased financial burden, and higher mortality rates. Midazolam, a commonly used benzodiazepine for sedation, can lead to acute withdrawal symptoms with acute restlessness, confusion, paranoid ideas, and hallucinations, if it is abruptly discontinued after prolonged use [11]. On the other hand, large doses of propofol can cause propofol infusion syndrome, a syndrome characterized by metabolic acidosis, muscle destruction, high lipid levels, and liver changes [12].Ketamine on the other hand acts as a dissociative anesthetic agent and is actually very effective in dissociating the central nervous system from the environment. It causes sedation and amnesia, analgesia but, on the other hand, maintains respiratory functions, cardiovascular stability, and airway reflexes. These properties, perhaps in association with anti-inflammatory and neuroprotective potential, may lead to improved management of symptoms, which can enable better cooperation with the patient [13].The cases presented in this series highlight the potential benefits of using ketamine in various critical care scenarios. It needs to be kept in mind, however, that the use of ketamine in critical care needs to be carefully monitored and managed in an individualized manner. Relevant side effects of high-dose continuous infusion ketamine use, like psychomimetic symptoms, hemodynamic instability, and increased intracranial pressure, need to be accounted for and managed with caution [14]. Any use of ketamine in critical care should be done on the basis of monitoring of vital signs, mental status, emergence of adverse effects, and dose adjustment or change in the mode of administration as indicated.
Limitations :
The major limitation of this case series is the fact that only six patients were included; hence, this series may thus not be representative of the critically ill population in general. Additionally, the lack of a control group makes it difficult to attribute the observed outcomes solely to ketamine, as other concurrent treatments may have influenced the results. Some bias in data collection or interpretation may have also resulted from its retrospective nature. Also, the generalizability of the results is reduced by diverse clinical conditions of the cases and different dosages of ketamine administered. The short-term follow-up itself makes it impossible to evaluate long-term effects and possible adverse outcomes from using ketamine in these patients. Further large-scale, randomized controlled trials are needed to validate these findings and establish standardized protocols for ketamine use in critical care settings
Conclusions
This case series contributes to a growing body of literature supporting the expanding role of ketamine in the critical care setting as a therapeutic agent with great potential value in a wide range of difficult clinical scenarios. However, in critically ill patients, use of ketamine needs to be tailored to the individual patient, with careful selection of the patient, titration of the dosage, and vigilance for possible adverse effects. Further studies are also needed before evidence-based recommendations can be formulated for the optimal use of ketamine in different critical care scenarios, as well as assessment of its long-term safety and efficacy in this patient population.
References
- Zorumski CF, Izumi Y, Mennerick S: Ketamine (2016). NMDA Receptors and Beyond: J Neurosci, 36:11164. 10.1523/JNEUROSCI.1547-16.2016
View at Publisher | View at Google Scholar - Kurdi MS, Theerth KA, Deva RS. (2014).: Ketamine: Current applications in anesthesia, pain, and critical care . Anesth Essays Res, 8:283-90. 10.4103/0259-1162.143110
View at Publisher | View at Google Scholar - Casamento A, Niccol T. (2022).Efficacy and safety of ketamine in mechanically ventilated intensive care unit patients: a scoping review. Crit Care Resusc J Australas Acad Crit Care Med, 7:71-82. 10.51893/2022.1.oa9
View at Publisher | View at Google Scholar - Orhurhu VJ, Vashisht R, Claus LE, Cohen SP. (2023). Ketamine Toxicity. StatPearls Publishing.
View at Publisher | View at Google Scholar - Goyal S., Agrawal A.(2013). Ketamine in status asthmaticus: a review . Indian J. Crit. Care Med, 17:154-161. 10.4103%2F0972-5229.117048
View at Publisher | View at Google Scholar - Uprety D, Baber A, Foy M. (2014). Ketamine infusion for sickle cell pain crisis refractory to opioids: a case report and review of literature. Ann Hemato, 93:769-71. 10.1007/s00277-013-1954
View at Publisher | View at Google Scholar - Rehder KJ . (2017).Adjunct Therapies for Refractory Status Asthmaticus in Children . Respir Care, 62:849-65. 10.4187/respcare.05174
View at Publisher | View at Google Scholar - Avidan MS, Maybrier HR, Abdallah AB, et al.(2017): Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery in older adults: an international, multicentre, double-blind, randomised clinical trial. Lancet Lond Engl, 15:267-75. 10.1016/S0140-6736(17)31467-31468
View at Publisher | View at Google Scholar - Fellous S, Dubost B, Cambriel A, Bonnet MP, Verdonk F. (2023): Perioperative ketamine administration to prevent delirium and neurocognitive disorders after surgery: a systematic review and meta-analysis. Int J Surg, 1:3555-3565. 10.1097/JS9.0000000000000619
View at Publisher | View at Google Scholar - Kress JP, Pohlman AS, O’Connor MF, Hall JB.(2000). Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med, 18:1471-7. 10.1056/NEJM200005183422002
View at Publisher | View at Google Scholar - Lerner A, Klein M: Dependence, withdrawal and rebound of CNS drugs: an update and regulatory considerations for new drugs development. Brain Commun. 2019, 1:025. 10.1093/braincomms/fcz025
View at Publisher | View at Google Scholar - Singh A, Anjankar AP: Propofol-related infusion syndrome: A clinical review . Cureus. 2022, 14:30383. 10.7759/cureus.30383
View at Publisher | View at Google Scholar - Umunna BP, Tekwani K, Barounis D, Kettaneh N, Kulstad E: Ketamine for continuous sedation of mechanically ventilated patients. J Emerg Trauma Shock. 2015, 8:11-5. 10.4103/0974-2700.145414
View at Publisher | View at Google Scholar - Radvansky BM, Shah K, Parikh A, Sifonios AN, Le V, Eloy JD: Role of ketamine in acute postoperative pain management: a narrative review. BioMed Res Int. 2015, 749837. 10.1155/2015/749837
View at Publisher | View at Google Scholar

 Clinic
Clinic
