Research Article | DOI: https://doi.org/10.31579/ 2835-8147/030
Healthcare Staff Experiences in Managing Responsive Behaviour of the Person with Dementia in Residential Care Facilities: A Qualitative Evidence Synthesis
1 Candidate Advanced Nurse Practitioner Memory Assessment and Support Service Woodhaven, First Sea Road, Sligo, Ireland.
2 Director of Nursing Plunkett Community Nursing Unit Boyle Ireland.
3 Senior Lecturer, School of Nursing and Midwifery, National University of Ireland, Galway, University Road, Galway, Ireland.
*Corresponding Author: Shiny Joy, Candidate Advanced Nurse Practitioner Memory Assessment and Support Service Woodhaven, First Sea Road, Sligo, Ireland.
Citation: Shiny Joy, Mary Butler, Maura Dowling (2023), Healthcare Staff Experiences in Managing Responsive Behaviour of the Person with Dementia in Residential Care Facilities: A Qualitative Evidence Synthesis, Clinics in Nursing, 2(4); DOI:10.31579/ 2835-8147/030
Copyright: © 2023, Shiny Joy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 12 July 2023 | Accepted: 19 July 2023 | Published: 25 July 2023
Keywords: responsive behaviour; dementia; qualitative evidence synthesis; vips model
Abstract
Background: Dementia is a collective term for all conditions that cause damage to the brain. Responsive behaviour is one of the symptoms of dementia trajectory and more than 90% of people with dementia present with responsive behaviour. These behaviours can adversely affect residents and staff in residential care services. There is a lack of understanding of how staff experience and manage responsive behaviours in residential settings.
Objective: This qualitative evidence synthesis aimed to explore the experiences and perceptions of healthcare staff in managing responsive behaviour of residents with dementia in older persons’ residential care services.
Methods: A systematic search across six databases was performed. A rigorous screening process, using inclusion/ exclusion criteria identified nine studies for synthesis. ‘Best- fit’ framework synthesis using the VIPS (Valuing, Individualised, Perspective, Social and psychological environment) framework guided synthesis.
Findings: This synthesis has revealed a new dimension of understanding responsive behaviours by illustrating the sub- themes of valuing residents and staff, knowing residents through life history, unmet needs, the perspective of institutionalised care practices, emotional distance, the importance of meaningful activities and a supportive environment.
Conclusion: This review has identified the importance of ensuring the accessibility to dementia-specific education to all staff and a supportive management structure to provide no-blame culture within the organisation.
Introduction
Dementia is a collective term for all conditions that cause damage to the brain and thereby affect the memory, thinking and cognitive functioning of the person (World Health Organisation (WHO), 2021). As dementia is a progressive disease, when the condition progresses, the behavioural and psychological symptoms of dementia (BPSD) like aggression, agitation and depression are common [17]. Residents’ aggression and violence in care settings can adversely affect both residents and staff. For staff, it creates a feeling of insecurity, staff burnout and emotional disturbances [14], and for residents, it results in poor quality of care and care relationships (Dupuis et al., 2016). Labelling a person with dementia as agitated and aggressive directly influences their personhood. The need-driven, dementia-compromised behaviour (NDB) theory highlights that, behaviours in dementia often labelled as challenging, develop from unmet needs [1]. Staff response to these behaviours depends on their understanding, attitude and view of people with dementia and their behaviours[8].
Aim
This qualitative evidence synthesis aimed to synthesise all available qualitative studies which explore the experiences and perceptions of healthcare staff in managing the responsive behaviour of residents with dementia in older persons’ residential care services.
Methods
Qualitative evidence synthesis enables the integration of isolated qualitative findings systematically to inform policymakers and improve the quality of care. The specific approach adopted was ‘best-fit framework synthesis’ (BFFS) (Booth and Carroll, 2015). The BFFS approach uses an a priori framework to guide analysis and synthesis. The EPOC (Effective Practice and Organisation of Care) statement [13] guided this review. The SPICE tool (Setting, Perspective, Phenomenon of interest, Comparison, Evaluation) was used to inform the search strategy (Table 1), develop search terms and create inclusion and exclusion criteria (Table 2).
Terms used for search strategies across databases, framed in the SPICE mnemonic.
Setting | Perspective | Phenomenon of Interest | Comparison | Evaluation |
| Older persons’ residential care services | Health care staff | Responsive behaviour management in dementia care | Caring for residents who have no dementia | Experience
|
Nursing Home Long-term care facility Assisted living services Residential homes Elderly Aged Geriatric Old Senior Residential care Assisted living Care home Long stay Aged* Old* Senior*
| Health care professionals Nursing staff Professional caregiver Formal care staff Staff nurses Nurses Care staff Professional health worker Caregiver Formal carers Healthcare assistants Healthcare workers | “Responsive Behaviour” “Challenging behaviour” “Disruptive behaviour” “Problem behaviour” “Rational behaviour” Violence Agitation Aggression Wandering Screaming Cursing Anxiety “Sexual inhibited behaviour” Restlessness “Behavioural and psycho social symptoms of dementia” BPSD | Dementia Alzheimer's disease Vascular dementia Lewy body dementia Parkinson’s disease Frontotemporal dementia Creutzfeldt-Jakob Mixed dementia Huntington’s disease
| Opinion Perception Views Knowledge Understanding Idea Satisfaction qualitative research" qualitativestudy* qualitative "qualitative method*" ethnograph ethnograf Phenomen* “Grounded theor*” interview* " focus group*" "lived experience*" observation* "purposive sampl*" perseptive* opinion* experience* narrat* Questionnaire “mixed method*” thematic* Descriptive* Lifeworld “Conversation analysis” “Action research” Hermeneutic “Content analysis” Colaizzi Heidegger Van Manen Merleau Ponty Husserl or Questionnaire |
Table 1: Inclusion/exclusion criteria
Inclusion Criteria
Setting and participants:
1. Studies conducted in long-term care facilities, which provide residential care for older people.
2. Studies focused on employed staff including healthcare assistants, nurses and other healthcare professionals those who experienced responsive behaviours exhibited by people with dementia living in long-term care homes.
3. Studies involving adult participants, aged above 18 years.
4. Responsive behaviours of any form of verbal, physical or sexual behaviours towards staff exhibited by people living in residential homes.
5. Primary data of health care staff experiences, perceptions, views and opinions of managing responsive behaviour of older persons with dementia.
Study designs:
1. Qualitative studies with primary data to include personal experiences or perceptions, interviews, direct observation, focus groups, participating action research, grounded theory, ethnography, content analysis, thematic analysis, narrative analysis, generic qualitative studies, phenomenology and case studies.
2. Studies that use mixed methods for data collection including focus group discussions, observations, interviews, dairies and open-ended survey questions.
3. Studies in the English language only.
Exclusion Criteria
1. Quantitative studies.
2. Studies not providing primary data such as literature reviews and integrative reviews.
3. Studies with languages other than English.
4. Studies with responsive behaviour of residents, those who have no dementia.
5. Experience of relatives or family members.
6. Studies conducted in acute hospital settings.
7. Studies conducted in residential homes admit primarily younger people.
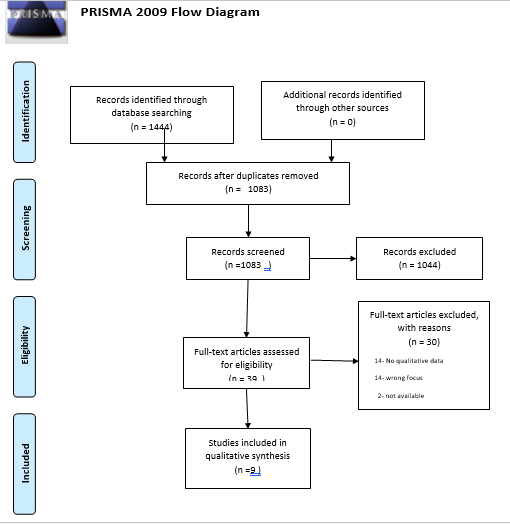
An experienced librarian assisted in developing a precise search strategy with all variations and combinations of keywords, MESH headings and subject headings in different databases. The searches across six databases CINAHL, PubMed, Medline, Embase, Psych INFO and ProQuest were completed in December 2020. Unpublished theses in the grey literature were also searched capturing the entire body of available studies and avoiding publication bias. (Table 3). The database searches identified a total of 1444 studies. An additional final search was performed in Google Scholar to ensure the rigorous searching process, but no further studies were identified. All studies were exported into the reference management software, Endnote X9. Following the removal duplicates in Endnote, 1,350 studies were imported into the Rayyan QCRI screening web application [19]. A Further 267 duplicates were removed from Rayyan. The title and abstract screening of all 1,083 studies were performed by the first and second authors, both with expertise in dementia care. Disagreements were resolved by the third author, who has experience in undertaking qualitative evidence syntheses. Following the full-text screening of 39 studies, 9 studies were included in the qualitative synthesis (Table 3). Quality assessment of the included 9 studies were carried out using the Critical Appraisal Skills Programme (CASP) framework. (Table 4). The VIPS (Valuing, Individualised, Perspective, Social and psychological environment) model of care was the framework used to guide synthesis. This model is recognised as the person-centred framework for people with dementia [16].
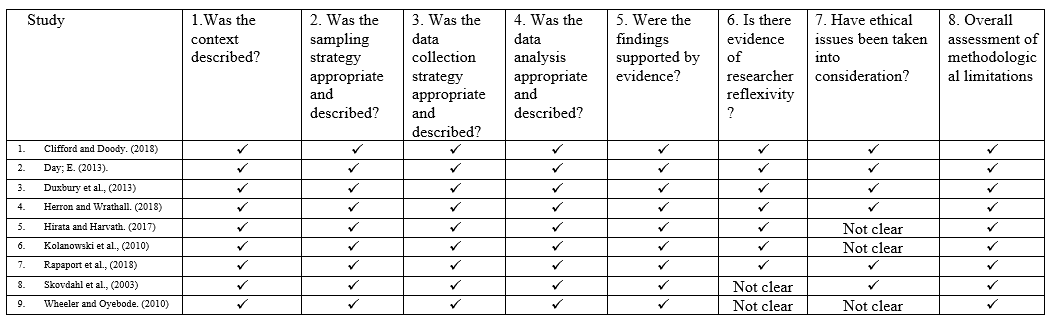
Table 3: CASP Table
No | Author, Year, Country | Design/Method | Sample & Sampling
| Analysis | Study Focus |
1 | Clifford and Doody. (2018)
Ireland
| Qualitative descriptive study | Purposive sampling of 9 nurses from public and private long-stay facilities. All nurses had the experience of responsive behaviours of dementia residents.3 staff nurses, 3 directors of nursing, 1 clinical nurse managers, and 2 assistant directors of nursing participated in the study. Semi-structured interviews were used to collect data. | Qualitative content analysis | This study focused to explore nursing staff attitudes of supporting people with dementia and responsive behaviours in residential care facilities. |
2 | Day, E. (2013)
England
| Qualitative study- Discourse analysis | Purposive convenient sampling- 12 paid care staff (6 from nursing home and 6 from residential home). A semi-structured interview was used to collect data from participants. | Foucauldian discourse analysis. | This descriptive study focused on examining the discourses that healthcare staff use to explain and describe challenging behaviour within dementia. |
3 | Duxbury et al., (2013)
United Kingdom
| Qualitative descriptive study | The study was carried out in four nursing homes in the North West of England, UK, that were owned by the same national company. 6 dementia care units in the homes and 1 unit were designated as a challenging behaviour unit. A convenience sample of staff 8 staff participated in the study (4- Dementia care unit managers, 2- nurses and 2- care assistants). Semi-structured was conducted to collect data from staff. Relatives- Focus Groups (2 groups) |
Thematic analysis | This study focused to explore the attitudes of nurses, and relatives regarding the causes of, and most effective ways of responding to aggressive behaviour from people with dementia in long term care settings. |
4 | Herron and Wrathall. (2018)
Canada
| Qualitative descriptive study | A purposive sample of 9 informal and 18 formal carers was recruited for the study. All participants experienced responsive behaviour of people with dementia. Among 18 formal carers; psych nurse- 6, RN- 9, LPN- 2, Nurse aid- 1 participated in the study. 27 semi-structured interviews were conducted to collect data. | Thematic analysis | This study focused to explore the views of formal and informal carers about the behaviours of people with dementia. It also focused to explore the network of social and physical environmental features of the place in which responsive behaviour of people with dementia take place. |
5 | Hirata and Harvath. (2017)
Japan
| A quantitative, cross-sectional, descriptive correlational study that included three open-ended questions. The answers to three open-ended questions were analysed using a qualitative content analysis | A convenience sample of 137 care workers from 10 special care units for persons with severe dementia in the nursing homes in the northern and western areas of Japan. Care workers who work full time only included in the study. Questionnaires were used to collect data. | Content analysis | This study focused to understand Japanese care workers’ beliefs, attributions and cultural explanations of physically and psychologically aggressive behaviour symptoms of people with dementia in residential care facilities. |
6 | Kolanowski et al., (2010)
United States
| Qualitative exploratory study
| A convenient sample of thirty-five staff members (registered nurses, licensed practical nurses, nurses’ aides, recreational therapists, activity personnel, and medical directors) from six nursing homes participated in the study. Focus group methodology was used to capture discussions. Each group size varied from 4-10 members. One hour group discussions were held in each facility. Discussions were audio-recorded and transcribed verbatim. | Content and thematic analysis. | This study focused to explore the need for cultural change in nursing homes. It also focused on drow out nursing, medical and recreational therapy staff attitudes of barriers to the application of nonpharmacological interventions for BPSD. |
7
| Rapaport et al (2018)
England
| Qualitative descriptive study | Purposive sampling of 25 care home staff of either sex, differing age, ethnicity, nationality and with different roles and experience were selected. Staff included are from six care homes in South East England including residential and nursing homes of differing sizes run by both the private and charity sector and located in urban and rural areas. Care assistant- 9, senior care assistant- 5, manager/deputy manager- 5, unit manager- 2, activity coordinator- 2, registered nurse- 2 Semi-structured interviews were conducted in their working place. | Thematic analysis | This study focused to understand residential care staff attitudes of how to respond and manage the agitation of residents with dementia |
8 |
Skovdahl et al., (2003)
Sweden |
Phenomenological-hermeneutic study
| Purposive sampling of 15 formal care staff from 3 care units was in the study. Unit one had residents with low-level agitation, unit 2 and 3 had residents with a high level of agitation.
Narrative interviews were performed to collect data to compare the narratives of two care groups. | Phenomenological-hermeneutic approach | This study focused on caregivers’ attitudes to behavioural and psychiatric symptoms of dementia (BPSD) and how do they experience the symptoms. |
9 | Wheeler and Oyebode (2010)
United Kingdom | Qualitative descriptive study | Focus groups were conducted with 36 direct care staff from nine care homes. Purposive sampling of staff including carers, nurses, activity coordinators and managers participated in the study. One hour focus group discussion was conducted in each nursing home to collect data. | Thematic analysis | This study focused to understand how care home staff manage challenging behaviour. To understand the extent to which care home staff have adopted person-centred care approach. |
Table 4: Study Characteristics
The VIPS acronym was developed by Dawn Brooker [4,6] (Table 6). It serves as a guide to ensuring the best care and quality of life for people with dementia through the organisational ethos and caring pathways. The primary data (participants’ verbatim accounts) and secondary data (observations, authors’ findings) were extracted by line-by-line coding and categorised into the selected four broad VIPS themes.
V: A value system that ensures the value of all individuals irrespective of cognitive impairment and age. I: Individualised approach P: View the world from the perspective of the affected persons S: Create a social environment that compensates for their impairment and support the Personhood of the person. |
Table 5: VIPS Framework [4,6]
Synthesis findings
The included 9 studies for synthesis were published from 2003-2018 and included a diverse range of healthcare staff. The findings are presented using
the VIPS framework, with inductive subthemes that were developed during synthesis. Table.7 illustrates themes and sub-themes.
Themes | Subthemes |
|
Valuing | Valuing the residents Valuing the staff | |
Individualised | Knowing the resident through life history Unmet needs | |
Perspective | Institutionalised care practices Emotional distance of staff members | |
Social | Importance of meaningful activities Supportive environment | |
Table 7: VIPS Themes and subthemes
Valuing
Valuing the residents
Staff understanding of responsive behaviour is clear “as a way of communicating” [8,14]. However, staff need thorough knowledge about a resident for interpreting the meaning of these communications [20]. Staff agree that the use of physical restraints is not necessary most of the time, and finding time to engage with residents is necessary to solve the problem [12]. However, when residents are extremely agitated staff tend to use chemical restraints sparingly not to be “drugging up” [12,23]. Various reasons for residents’ agitation and aggression have been identified by staff. These are mainly due to invading their personal space, stress from their inability to express their needs, the way staff interact with them and as a protective defence method when they couldn’t understand what happening around them [8,10,12,15]. Even though staff were aware of the responsive behaviours because of dementia, they tended to spend less time and tried to minimize interactions with those residents [15]. Residents’ aggressive behaviour is one of the reasons for some staff changing their caring methods. [15].stated that even though staff look after the residents with aggression, some staff treat the residents with agitation “coldly”. It was noticed the deputy manager’s concern about meeting the budget, therefore sometimes they needed to cut short staff and “the needs of the residents take second place” [20]. In big nursing homes with a large number of residents, the management’s focus was to filling their beds; “It is just a conveyor belt” [20].
Valuing the staff
Staff demonstrated their role in supporting residents with dementia by showing empathy, compassion and connecting with residents’ personhood [8,20]. They explained that the availability of resources and support from management determined their ability to support residents. ‘Staffing level’ and ‘skill mix’ play an important role to determine the time they can spend with each resident [8]. However, when they were short-staffed, they felt their “hands are tied off”[8]. Staff frequently expressed feelings of powerlessness and fear of being harmed especially when residents hit and shouted at staff [8,20]. Managing responsive behaviour by providing person-centred care demands more time and inclusion of multi-disciplinary team members including family members [8]. Staff expressed the feeling of being devalued and not being heard by managers when they expressed concerns [20,22] and, “they could be scared themselves” [8]. Staff acknowledged that they were unequipped and insecure to anticipate and deal with BPSD due to their lack of knowledge [8,10,17]. Lack of skills and knowledge resulted in staff attempting interventions such as a trial-and-error approach, eventually resulting in staff burnout and exacerbated institutional violence. Staff with specific training showed greater confidence and job satisfaction while managing responsive behaviours [22]. Staff without dementia training perceived that caring for the person with responsive behaviour is “difficult to manage”, they felt “fed up” and their work was “frustrating” [10,22,23]
Individualised
Knowing the resident through life history
The ability of staff to understand the moment in which the resident is living at that particular time and supporting them by ‘playing along’ is ideal rather than re-orient them [17,20]. However, staff felt uncomfortable lying to residents as they felt it may increase confusion [20]. Staff reported that the ‘life story work’ of each individual with dementia was hugely important to understanding their behaviour [8]. Consequently, new staff members and agency workers need more time to know each resident and their life stories to help them [8].
Unmet needs
Unmet needs are a major trigger of responsive behaviours of residents with dementia [8,12,20]. Availability of one-to-one time is hugely important to understand “what exactly is the reason for responsive behaviour that particular time” [8]. Characteristically, residents in the care home have a physical impairment that disables them to carry out daily activities. When cognitive and physical impairment are combined, staff prioritise residents’ safety issues and physical needs [17,20]. In such a way residents' emotional needs may be neglected [17]. Good interactions with residents and the communication skills of staff are essential to find out residents’ needs. However, it is vital to know to “back- off” when somebody is aggressive rather than arguing and compelling a resident [12]. Staff expressed their opinion as every person who works with residents with dementia must be fully committed as it states “really put 100% to know their residents’ characteristics” [12]. Staff sometimes single out residents as “reactive residents” thereby they consider residents’ identity as fixed and not capable of growing [14]. Conversely, some other staff believe unmet needs such as lack of stimulation and loneliness are the reason for these behaviours [14,20]
Perspective
Institutionalised care practices
Staff expressed their concern about struggling to finish their routines and the heavy workload in the care homes [10]. They aim to deliver a hierarchy of needs, therefore, basic care needs like washing, feeding and toileting are always considered the priority [20]. To keep routines, residents may need to “follow lots of orders” from staff [12]. Staff may have a fear of being blamed or getting into trouble, they give more importance to residents’ appearance over minimising distress, therefore, they insist residents get washed and changed [20]. Consequently, staff only focus on the physical aspects of care by invading residents’ personal space, and this results in residents’ responsive behaviours[12]. However, staff were afraid to try flexible approaches as they felt they were being blamed for neglecting residents’ care [20].
Emotional distance of staff members
Staff description of dementia and responsive behaviours showed a lack of understanding and emotional distance [10]. Day’s (2014) study highlighted that behaviour changes occur due to the separation of the body and mind of the affected person as: “it’s like you’re dead alive” [10]. The comparison of residents with dementia as ‘non-healthy’ and staff as ‘healthy’ indicates a widening emotional and dialectical gap [10]. It was also noticed that staff tend to place responsive behaviours in a disempowering position and try to avoid the blame from them by explaining it as “unpredictable” and “unprovoked” [10]. Staff highlighted matching personalities is essential to manage responsive behaviours [8].
Social
Importance of meaningful activities
Making people feel at home through various dementia-specific activities and a comfortable environment is therapeutic [20]. The availability of an activity coordinator and an individualised activity programme was identified as a good intervention to support and stimulate people with dementia [8,20]. Collaborating the works of the activity coordinator with residents’ care plans ensures person-centred care. Cross-training staff as both care assistants and activity personnel ensure the availability of skilled staff throughout [17]. Staff explained the difficulty of initiating activities to those who have no interests or specific hobbies [8].
Supportive environment
Staff identified both overstimulation and lack of interactions as reasons for residents’ distress [20]. The environmental “triggers” like noise, light, temperature, packed areas and time of the day play a role in a resident’s behaviour [10,14]. A quiet room with enough space to walk around and sit down, along with different options of activities to choose resulted in less agitation in care homes [12]. It was emphasised matching the personalities of residents when they share communal areas like the dining room can encourage residents’ social interactions [14]. Organisational factors like “shift change” escalates wandering and “exit–seeking” behaviours [14]. The overall design of the care home such as too many lounges, loud noise from the TV, moving residents in and out to the dining room, create lots of stimuli and increases conflicts [14]. Staff described care homes that evoke the image of ‘imprisonment’ for residents and they felt ‘trapped’ and unable to escape [20]. The care home environment itself is a trigger for resident-to-resident aggression, especially for residents with dementia [12].
Discussion
The responsive behaviours displayed by residential home residents with dementia are complex. Multiple personal, interpersonal and environmental factors are associated with the onset of these behaviours [17]. Even in the same resident, the triggering factors are varied in different occurrences. Residents with dementia dictate more demands on staff [17] and unmet needs are the prime reason for these behaviours. It is known that unmet physical needs such as ruling out pain and infections are under detected in residents with severe dementia [16,18]. That in turn increases the occurrences of responsive behaviour. However, the best way to support residents with dementia is to value them as unique individuals [22]. The importance of developing a good care relationship while caring for people with dementia through empathy, gentle approaches and interpersonal communications are highlighted [14]. Staff felt frightened and powerless when labelling behaviours as challenging or problematic [20]. For care staff to achieve competence, they need genuine interest and knowledge about residents in their care as well as a thorough theoretical understanding of dementia and responsive behaviour [22]. Conversely, lack of competency contributes to staff feeling afraid of residents with dementia and responsive behaviours [22]. Therefore, it is not about a greater number of staff, it’s about the right staff with a positive attitude, training and experience [17,20,23]. The provision of person-centred care in a residential home hugely depends on the family-staff partnership and the involvement of the multi-disciplinary team [17]. It is important to address any problems when they develop and seek wider team support before they worsen [23]. Valuing the person with dementia as well as care staff determines the success of person-centred care (Kitwood, 1997). Therefore, care staff should have a supportive work environment rather than an environment where blame is apportioned to care staff. Any provoking incidents like hygiene care needs should be handled carefully [12]. Various individualised de-escalation and distraction techniques need to be identified to deal with responsive behaviour promptly by involving a multi-disciplinary team. However, it was recognised that wherever staff had a poor understanding of the importance of psychosocial interventions, medication management is the prime way of managing responsive behaviour [23]. The physical environment of the person with dementia living in residential care contributes a major role to their behaviour. Herron and Wrathall (2018) It is argued that the problems and solutions to residents’ responsive behaviour are mostly associated with the system of care and structure of the place they are living [14].
Implications for clinical practice
The findings of this qualitative evidence synthesis highlight the importance of dementia-specific education. It is essential to provide continuing education to all staff working in older person’s services. This will promote greater self-awareness, personal growth and positive interpersonal relationships between care staff and residents with dementia.
Study strength and limitations
One of the limitations of this study is that the focus is only on the voice of the healthcare staff and the views and feelings of residents and residents’ relatives have not been captured. The concerns of the person with dementia and their families also need to be considered in decision-making regarding their care needs and responsive behaviours.
Conclusion
The success of responsive behaviour management and person-centred care relies on the right caring staff with the right education and good attitude [17]. Staff self-awareness, with a compassionate and empathetic approach, makes residents feel valued. Supportive management is crucial to ensure the well-being of residents and staff. This study has revealed new dimensions of care to manage responsive behaviour. Qualitative evidence synthesis methodology was used to illustrate the dimensions of managing responsive behaviours and using the VIPS framework aided this work. The authors hope these findings can be communicated to all care home staff and training institutions responsible for the education and training of staff to manage responsive behaviour respectfully.
References
- Algase D.L., Beck C., Kolanowski A., Whall A., Richards, K., et al., (1996). Need-driven dementia-compromised behavior: An alternative view of disruptive behavior. American Journal of Alzheimer’s Disease and Other Dementias, 11 (6), 10-19.
View at Publisher | View at Google Scholar - Booth A., and Carroll, C. (2015). How to build up the actionable knowledge base: the role of ‘best fit’ framework synthesis for studies of improvement in healthcare. BMJ quality & safety, 24(11), pp.700-708.
View at Publisher | View at Google Scholar - Brooker, D. (2004). What is person-centred care for people with dementia? Rev. Clin. Gerontol. 13 (3), 215-222.
View at Publisher | View at Google Scholar - Brooker, D. (2006). Person-Centred Dementia Care: Making Services Better. Jessica Kingsley Publishers, London.
View at Publisher | View at Google Scholar - Brooker, D. (2012). Understanding dementia and the person behind the diagnostic label. Int. J. Pers. Cent. Med. 2 (1), 11-17.
View at Publisher | View at Google Scholar - Brooker, D. and Lantham, I. (2016). Person-Centred Dementia Care. Making Services Better with the VIPS Framework. Jessica Kingsley Publishers, London.
View at Publisher | View at Google Scholar - Brooker, D.J., Woolley, R.J. and lee, D. (2007). Enriching opportunities for people living with dementia in nursing homes: An evaluation of a multi-level activity-based model of care. Aging Ment. Health. 11, 361-370
View at Publisher | View at Google Scholar - Clifford, C. and Doody, O. (2018). Exploring nursing staff views of responsive behaviours of people with dementia in long‐stay facilities. Journal of psychiatric and mental health nursing, 25(1), pp.26-36.
View at Publisher | View at Google Scholar - Carroll, C., Booth, A., Leaviss, J. and Rick, J. (2013). “Best fit” framework synthesis: refining the method. BMC medical research methodology, 13(1), pp.1-16.
View at Publisher | View at Google Scholar - Day; E. (2013). “It’s like you ’re dead alive”. How do professional care staff construct challenging behaviour amongst residential and nursing home residents living with dementia”. A discourse analysis approach. (Doctoral dissertation, University of Surrey).
View at Publisher | View at Google Scholar - Dupuis, S., Mc Ainey, C.A., Fortune, D., Ploeg, J. and Witt, L.D. (2016). Theoretical foundations guiding culture change: The work of the Partnerships in Dementia Care Alliance. Dementia, 15(1), pp.85-105.
View at Publisher | View at Google Scholar - Duxbury, J., Pulsford, D., Hadi, M. and Sykes, S. (2013). Staff and relatives' perspectives on the aggressive behaviour of older people with dementia in residential care: a qualitative study. Journal of psychiatric and mental health nursing, 20(9), pp.792-800.
View at Publisher | View at Google Scholar - Glenton, C., Bohren, M.A., Downe, S., Paulsen, E. and Lewin, S. (2019). EPOC qualitative evidence synthesis: protocol and review template, EPOC Resources for review authors. Oslo: Norwegian Institute of Public Health. (online).
View at Publisher | View at Google Scholar - Herron, R.V. and Wrathall, M.A. (2018). Putting responsive behaviours in place: Examining how formal and informal carers understand the actions of people with dementia. Social Science & Medicine, 204, pp.9-15.
View at Publisher | View at Google Scholar - Hirata, H. and Harvath, T.A. (2017). Japanese care workers’ perception of dementia‐related physically and psychologically aggressive behaviour symptoms. International journal of older people nursing, 12(1), p.e12119.
View at Publisher | View at Google Scholar - Husebo, B.S., Ballard, C., Cohen-Mansfield, J., Seifert, R. and Aarsland, D. (2014). The response of agitated behavior to pain management in persons with dementia. The American Journal of Geriatric Psychiatry, 22(7), pp.708-717.
View at Publisher | View at Google Scholar - Kolanowski, A., Fick, D., Frazer, C. and Penrod, J. (2010). It's about time: use of nonpharmacological interventions in the nursing home. Journal of Nursing Scholarship, 42(2), pp.214-222
View at Publisher | View at Google Scholar - Kovach, C.R. (2013). Assessing pain and unmet need in patients with advanced dementia: the role of the Serial Trial Intervention (STI). In Handbook of pain and palliative care (pp. 131-144). Springer, New York, NY.
View at Publisher | View at Google Scholar - Olofsson, H., Brolund, A., Hellberg, C., Silverstein, R., Stenström, K., Österberg, M., & Dagerhamn, J. (2017). Can abstract screening workload be reduced using text mining? User experiences of the tool Rayyan. Research Synthesis Methods, 8(3), 275-280. doi:10.1002/jrsm.1237
View at Publisher | View at Google Scholar - Rapaport P., Livingston G., Hamilton O., Turner R., Stringer,A., et. Al., (2018). How do care home staff understand, manage and respond to agitation in people with dementia? A qualitative study. BMJ open, 8(6),.
View at Publisher | View at Google Scholar - Røsvik J., Kirkevold M., Engedal K., Brooker D. and Kirkevold, Ø. (2011). A model for using the VIPS framework for person‐centred care for persons with dementia in nursing homes: a qualitative evaluative study. International journal of older people nursing, 6(3), pp.227-236.
View at Publisher | View at Google Scholar - Skovdahl, K., Kihlgren, A.L. and Kihlgren, M., (2003). Different attitudes when handling aggressive behaviour in dementia--narratives from two caregiver groups. Aging & Mental Health, 7(4), pp.277-286.
View at Publisher | View at Google Scholar - Wheeler, N.L. and Oyebode, J.R., (2010). Dementia care. 2: Exploring how nursing staff manage challenging behaviour. Nursing times, 106 (25), pp.20-22.
View at Publisher | View at Google Scholar - World Health Organisation (WHO), (2021). Dementia. (Online).
View at Publisher | View at Google Scholar

 Clinic
Clinic
