case Report | DOI: https://doi.org/10.31579/2835-835X/101
Employing Amniotic Membrane Allografts As A Regenerative Treatment For Burn Injuries
1Shanmuga Priya R, Senior Resident, Department of Plastic Surgery, Jawaharlal Institute of Post graduate Medical Education and Research (JIPMER), Pondicherry, India.
2Professor & Registrar (Academic), Head of IT Wing and Telemedicine, Department of Plastic Surgery & Telemedicine, JIPMER, Pondicherry, India.
3Siddu C, Department of general surgery, Jawaharlal institute of post graduate medical education and research (JIPMER), Pondicherry, India.
*Corresponding Author: Ravi Kumar Chittoria, Professor & Registrar (Academic), Head of IT Wing and Telemedicine, Department of Plastic Surgery & Telemedicine, JIPMER, Pondicherry, India.
Citation: Shanmuga Priya R, Ravi K. Chittoria, Siddu C, (2025), Employing Amniotic Membrane Allografts As A Regenerative Treatment For Burn Injuries, Clinical Trials and Case Studies, 4(1); DOI:10.31579/2835-835X/101
Copyright: © 2025, Ravi Kumar Chittoria. This is an open-access artic le distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 15 January 2025 | Accepted: 03 February 2025 | Published: 24 February 2025
Keywords: amniotic membrane allograft; wound healing; regenerative therapy
Abstract
Burn injuries affect individuals of all ages and can be caused by thermal, scald, or electrical sources. Various scaffolds are currently used to support the healing process and reduce scar formation. Collagen acts as a scaffold by promoting tissue regeneration and encouraging the development of new blood vessels. Similarly, scaffolds like the amniotic membrane support proper epithelialization and minimize scarring while offering unique anti-inflammatory and bacteriostatic benefits. In this study, we applied an amniotic membrane allograft as a biological dressing for burn wounds on the right thigh of an adult patient.
Introduction
Wound healing is a biological process that responds to various forms of injury, including physical, chemical, mechanical, or thermal damage. This process unfolds through several distinct stages: hemostasis, inflammation, proliferation/granulation, and remodeling/maturation [1]. However, deviations from the normal healing pathway, such as prolonged inflammation, are commonly observed in burn injuries, where typical healing mechanisms may be impaired [2]. Modern medicine has increasingly turned to scaffolds, both natural and synthetic, to address these challenges. An ideal scaffold should meet several criteria: suitable physical and mechanical properties, a physiological environment that supports cellular adhesion, proliferation, and differentiation, high porosity, a favorable surface area-to-volume ratio, flexibility to adapt to wound contours, and biocompatibility and biodegradability [3].
Collagen, whether derived naturally or synthetically, serves as an effective dermal matrix substitute, aiding epithelialization during wound repair [4]. Additionally, the breakdown of collagen promotes neovascularization and supports angiogenesis. The amniotic membrane, a natural scaffold, possesses unique properties, including anti-inflammatory, bacteriostatic, anti-fibrotic, anti-scarring, and epithelialization-enhancing effects [6]. Its low immunogenicity and the presence of progenitor cells make it a highly promising option for use as a scaffold in wound healing. Silicone, on the other hand, acts as a protective barrier, reducing mechanical friction and transepidermal water loss—factors associated with infection severity. Research suggests that silicone may influence inflammatory growth factors involved in fibrosis and facilitate acute wound healing by regulating key markers such as TNF-α, TGF-β, IL-1, and IL-6.
Materials and Methods
This study was conducted in the Department of Plastic Surgery at a Tertiary Care Center following approval from the institutional ethical committee. Written informed consent was obtained from the patient. The subject of this study was a 42-year-old male who presented with a residual non-healing raw area on the left leg, 70 days after sustaining thermal burns.
Upon admission to the specialized burn care unit, the patient received initial management, including intravenous fluids, analgesics for pain control, and prophylactic antibiotics. As part of regenerative wound therapy, a three-layered scaffold dressing was prepared and applied to the affected area. This dressing included a sterile amniotic membrane, placental extract, and a silicone sheet, with the amniotic membrane placed directly in contact with the wound bed.
The amniotic membrane, obtained from a freshly delivered placenta, was thoroughly cleaned (figure 1), processed, and stored in an antibiotic solution under refrigeration until use The scaffold (Figure. 2).
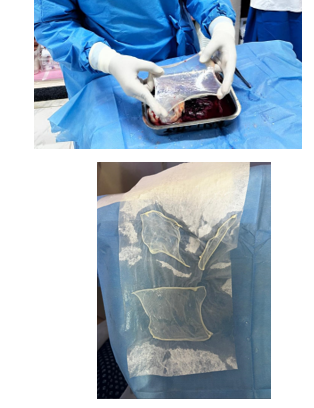
Figure. 2-Dressing was left in place for seven days. During this period, the amniotic membrane was fully absorbed, and the silicone sheet was removed, revealing significant wound healing progress.
Results
The patient experienced an uneventful intraoperative and postoperative course. Upon removing the dressing on the seventh day after the procedure, significant re-epithelialization and wound healing were observed. All second-degree superficial burn wounds healed completely without any complications or adverse effects throughout the treatment.

Figure-3-The BJWAT wound score improved notably from 32 at initial presentation to 20 following the application of regenerative therapy using the amniotic membrane.
Discussion
Partial-thickness burn injuries generally have the capacity to heal spontaneously, whereas full-thickness burns often require skin grafting to achieve complete wound closure. Traditionally, split-thickness skin autografts have been the standard treatment for closing excised full-thickness burn wounds [5]. However, in cases of extensive burns, the availability of sufficient donor sites for autograft harvesting can be a significant limitation. This has led to the exploration of alternative approaches, such as skin substitutes.
Engineered skin substitutes provide temporary wound coverage until donor sites become available for autografting or, when incorporating autologous cells, may offer permanent closure [7]. Although the development of permanent skin substitutes remains limited, ongoing advancements in tissue engineering are expected to improve available options for burn wound management. For example, the Dermal Regeneration Template, a commercially available product, consists of a two-layered system. Its outer layer is a thin silicone film that serves as a protective barrier, minimizing infection risks and regulating heat and moisture loss. The inner layer, made of a collagen-glycosaminoglycan (GAG) matrix, acts as a biodegradable scaffold that supports dermal tissue regeneration. The porous structure of the template facilitates skin regeneration by providing a framework for new tissue growth. Once the dermal layer regenerates, the outer silicone layer is replaced with a thin epidermal skin graft, enabling permanent skin regeneration, accelerating wound healing, and reducing scarring.
Inspired by this mechanism, we developed a cost-effective dermal regeneration scaffold using a combination of a silicone sheet, dry collagen sheets, and amnion. This indigenous scaffold is particularly suited for use in hospital settings in developing countries, where the high cost of commercial dermal regeneration templates may be prohibitive. It provides an affordable and practical alternative for promoting wound healing and tissue regeneration.
Conclusion
This study demonstrates the effectiveness of using a cost-efficient regenerative scaffold dressing, based on amniotic membrane, in treating second-degree scald burns. The treatment significantly accelerates the healing process of both superficial and deep second-degree wounds, reducing healing time to less than a week and minimizing hospitalization duration and infection rates. However, additional large-scale, multicenter, double-blinded controlled trials with statistical analysis are needed to further validate these findings.
References
- Haghpanah S, Bogie K, Wang X, Banks PG, Ho CH. (2006). Reliability of electronic versus manual measurement techniques. Arch Phys Med Rehabil. 87: 1396-1402.
View at Publisher | View at Google Scholar - Chitoria RK, Kumar P, Baljaj SP, Singh AK, Gupta DK. (2014). General clinical guidelines for wound management: Redefining acronym SWCR. Journal of SWCR.;7(1): 2-7.
View at Publisher | View at Google Scholar - Shetty R, Sreekar H, Lamba S, Gupta AK. (2012). A novel and accurate technique of photographic wound measurement. Indian J Plast Surg.; 45(2): 425- 429.
View at Publisher | View at Google Scholar - Majeske C. (1992). Reliability of wound surface area measurement. PhyTher.; 72: 138-141.
View at Publisher | View at Google Scholar - Mayrovitz HN, Soontupe LB. (2009). Wound area by computerized planimetry of digital images. Adv Skin Wound Care.; 22: 222-229.
View at Publisher | View at Google Scholar - Pandey S, Chitoria RK, Mohapatra DP, et al. (2016). Application of digital planimetry: A novel technique of wound measurement in diabetic foot ulcer. Dermatology International.; 21: 343-331.
View at Publisher | View at Google Scholar - Pires IM, Garcia NM. (2015). Wound area assessment using mobile application. Proceedings of the International Conference on Biomedical Electronics and Devices - SmartMedDev, International Conference on Biomedical Elechonics and Devices; 12- 15; pp. 271-282.
View at Publisher | View at Google Scholar

 Clinic
Clinic
