case report | DOI: https://doi.org/10.31579/2835-7957/095
Dangerous Miss- An Unusual Case of Pain in Abdomen
- Rajeev Bhardwaj *
- Sivaji Patibandla
- Gaurav Aggrawal
- Mehroj Mirza
Department of Cardiology, MM Institute of Medical Sciences and Research, Mullana, Ambala (India)
*Corresponding Author: Da-Yong Lu, School of Life Sciences, Shanghai University, Shanghai 200444, PRC.
Citation: Rajeev Bhardwaj., Sivaji Patibandla., Gaurav Aggrawal., Mehroj Mirza, (2024), Dangerous Miss- An Unusual Case of Pain in Abdomen, Clinical Reviews and Case Reports, 3(5); DOI:10.31579/2835-7957/095
Copyright: © 2024, Rajeev Bhardwaj. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 19 August 2024 | Accepted: 29 August 2024 | Published: 04 September 2024
Keywords: superior mesenteric artery; ischemia; angioplasty; stenting
Abstract
Abdominal pain is a common complaint in patients coming to emergency services as well as in patients coming to medicine and surgical outpatient departments (OPD). Sometimes in spite of exhaustive workup, the diagnosis may not be made, which is very troublesome for the patient as well as for the physician. We present one such case, who remained undiagnosed for more than eight years.
Case:
66 years male presented with pain in upper abdomen for the last 10 years. Pain was moderate in intensity initially, used to occur 20-30 minutes after meals. It lasted for around 30 minutes. After the pain, patient used to have vomiting and he got relief from pain. The intensity of pain increased over the years. Around one year before his symptoms, he was operated for some abdominal compliant, but there was no record of it. For three years, he used to be admitted 1-2 times a year in surgery department with pain in abdomen, vomiting and some constipation. Diagnosis each time was sub acute intestinal obstruction. He used to be treated conservatively, with ryles tube aspiration and intra venous fluids and was kept nil per orally (NPO). He used to be relieved and discharged after 7-8 days. After this he visited many hospitals with at least 5 more admissions. During his stay in hospitals, his ultra sound, upper gastro intestinal (GI) endoscopy, and colons copy was done few times and was normal each time. His coronary angiography was done, with possibility of post prandial angina and was normal. For the last two months he was on liquid diet only and had lost 14 kg weight in last two months.
Upper GI endoscopy: Doudenal bulb showed clean based ulcer.
Enterography : Suspicion of superior mesenteric artery (SMA) disease.
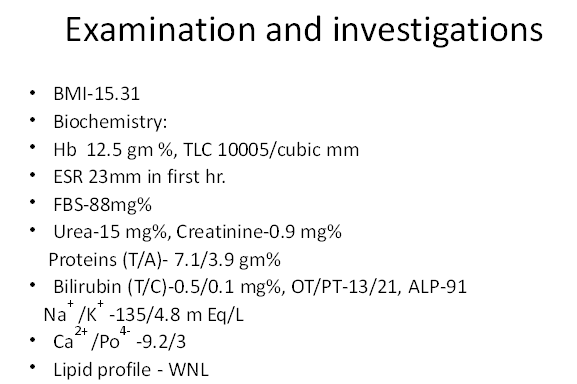
CT angio of abdomen: severe ostial stenosis of SMA. There was reformation of distal SMA from collaterals from gastro duodenal artery. Angle between aorta and SMA was 19.4 degree.
Patient was taken up for angioplasty of SMA through left brachial approach. Judkin’s right, 7F catheter was taken to hook SMA. Selective angiography of SMA showed ostial stenosis of SMA (Figure 2) Whisper wire was crossed. Ostium of SMA was dilated with 3x12 mm balloon (Figure 3). Lesion was very hard. Stent of 5 mm was implanted (Figure 4). There was no residual stenosis Figure 5)
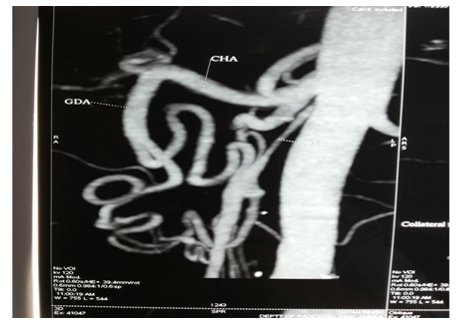
Figure 1: CT angio of abdomen shows severe ostial stenosis of SMA, with filling of distal SMA from collateral arising from GDA.
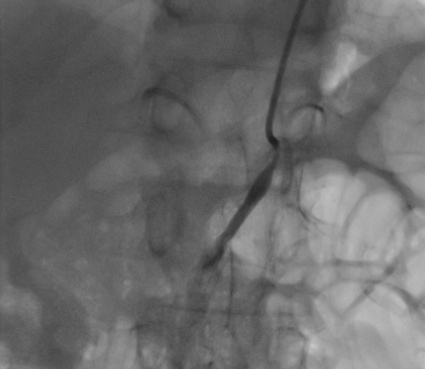
Figure 2: Selective angiography of SMA shows severe stenosis of ostium of SMA. Distal SMA is not seen.
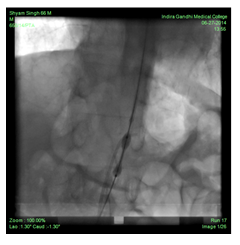
Figure 3: Dilatation of SMA with balloon. Waist in balloon shows the hardness of lesion.
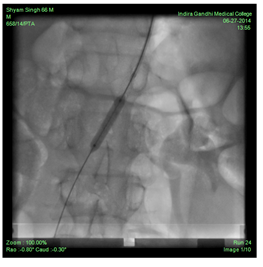
Figure 4: Stent implantation in SMA

Figure 5: Final result after stenting.
That day patient could take solid food after 2 months. There was no pain in abdomen after the meals. Patient was discharged after two days. He continued to be asymptomatic. After 2 months, he had gained 5 kg weight.
Discussion:
Mesenteric ischemia has the potential for being acutely life threatening or a debilitating chronic illness. Few endovascular specialists have significant experience with the visceral or mesenteric vascular bed. Barriers to treatment can include a lack of knowledge of the anatomy, physiology, and treatment approaches. Mesenteric blood supply comes from three main arterial vessels which arise from the aorta beginning just below the diaphragm and ending above the aortic bifurcation. These are celiac artery (CA), superior mesenteric artery (SMA) and inferior mesenteric artery (IMA). For symptoms to occur, it is classically taught that two out of three vessels need to be occluded, with the third compromised. This is certainly not the case when compromise occurs acutely and collaterals have not been established. Furthermore, there are symptomatic cases in which a single vessel (typically the SMA) is chronically stenosed. These may be evident when previous abdominal operations have disrupted the collaterals or after surgical abdominal aortic aneurysm repair. The primary vascular process affecting the mesenteric vessels is atherosclerosis, typically at the aorto-ostial junction. The frequency and extent of atherosclerotic narrowing are much greater than the incidence of symptomatic disease. Asymptomatic patients with multiple-vessel involvement generally are at the greatest risk of becoming symptomatic, and approximately one-third of these individuals may progress to frank intestinal infarction [1]. Chronic mesenteric ischemia (CMI) may occur from either postprandial shunting of blood to the gastric circulation or from demand ischemia [2]. Patients are typically elderly cachectic women who have undergone a panel of tests before the diagnosis is ultimately made. Beyond the universal complaint of postprandial abdominal pain, patients may also present with complaints suggesting gastropathy or colitis. A high index of clinical suspicion is important for making a timely diagnosis of chronic mesenteric ischemia, which is often delayed as patients are often first evaluated for other etiologies (especially malignancy) as an explanation for weight loss. The average delay from the beginning of symptoms to diagnosis or treatment was 10.7 months in one review 3 and 15 months in another [4]. Mesenteric angioplasty and stenting have become a first-line therapy for patients with chronic mesenteric ischemia. Stenting the superior mesenteric or celiac artery has high technical and early clinical success rates. Most authors have reported technical success rates of greater than 80 percent, and relief of abdominal pain occurs in 75 to 100 percent of patients, with one half of patients experiencing weight gain [4,5,6]. Our patient was unusual in the sense that diagnosis was delayed for many years. Patient underwent detailed diagnostic work up for abdominal pain in many hospitals but mesenteric ischemia was never thought as a possibility. Patient had only SMA involvement. Probably previous abdominal surgery had damaged the collaterals.
References
- Kolkman JJ, Mensink PB, van Petersen AS, et al. (2004). Clinical approach to chronic gastrointestinal ischaemia from “intestinal angina” to the spectrum of chronic splanchnic disease. Scand J Gastroenterol Suppl.241:9-16.
View at Publisher | View at Google Scholar - Poole JW, Sammartano RJ, Boley SJ.(1987). Hemodynamic basis of the pain of chronic mesenteric ischemia. Am J Surg. 153:171-176.
View at Publisher | View at Google Scholar - Pecoraro F, Rancic Z, Lachat M, et al. (2013). Chronic mesenteric ischemia: critical review guidelines for management. Ann Vasc Surg. 27:113.
View at Publisher | View at Google Scholar - Silva JA, White CJ, Collins TJ, et al. (2006). Endovascular therapy for chronic mesenteric ischemia. J Am Coll Cardiol; 47:944.
View at Publisher | View at Google Scholar - Aburahma AF, Campbell JE, Stone PA, et al. (2013). Perioperative and late clinical outcomes of percutaneous transluminal stentings of the celiac and superior mesenteric arteries over the past decade. J Vasc Surg ; 57:1052.
View at Publisher | View at Google Scholar - Kougias P, El Sayed HF, Zhou W, Lin PH. (2007). Management of chronic mesenteric ischemia. The role of endovascular therapy. J Endovasc Ther; 14:395.
View at Publisher | View at Google Scholar

 Clinic
Clinic
