case report | DOI: https://doi.org/10.31579/2835-7957/074
Clinical Observation and Nursing Experience of Carotid Endarterectomy after Carotid Artery Stenosis Caused by Atherosclerosis
- Min Dong
- Wang Xiao-Dong *
Department of Rehabilitation Medicine, Inner Mongolia Autonomous Region People's Hospital, Hohhot, China.
*Corresponding Author: Wang Xiao-Dong, Department of Rehabilitation Medicine, Inner Mongolia Autonomous Region People's Hospital, Hohhot, China.
Citation: Min Dong, Wang X. Dong, (2024), Clinical Observation and Nursing Experience of Carotid Endarterectomy after Carotid Artery Stenosis Caused by Atherosclerosis, Clinical Reviews and Case Reports, 3(2); DOI:10.31579/2835-7957/074
Copyright: © 2024, Min Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: 14 March 2024 | Accepted: 20 March 2024 | Published: 29 March 2024
Keywords: atherosclerosis; carotid stenosis; carotid endarterectomy(cea)
Abstract
At present, cerebral infarction has become a serious disease that endangers human health, and one of the important reasons for cerebral infarction is carotid artery stenosis. Carotid Endarterectomy (CEA) is a surgical procedure to treat carotid artery stenosis, its principle is to remove carotid plaque and relieve carotid artery stenosis, thereby increasing the distal cerebral blood supply and preventing cerebral infarction. Carotid endarterectomy was first performed on patients in 1953 by Professor De Bakey of vascular surgery and has been used for more than 70 years. Due to its effectiveness in the treatment of carotid artery stenosis, it has become an important routine operation in neurosurgery and cerebrovascular department, greatly reducing the risk of stroke in patients. In particular, a large number of clinical trials were represented by the North American Endarterectomy Trial for Symptomatic Carotid Stenosis (NASCET) [1], the European Carotid Surgery Trial (ECST) [2], the Asymptomatic Carotid Stenosis versus Aspirin Trial (CASANOVA) [3], and the Asymptomatic Carotid Surgery Trial (ACST) [4]. After the results of the bed trial were published successively, the effective role of CEA in the treatment of carotid atherosclerotic stenosis became more clearer, and the status of CEA was further consolidated. This paper reports a case of carotid endarterectomy and reviews the relevant literature.
Introduction
Carotid endarterectomy (CEA) is a surgery for the treatment of carotid artery stenosis. It works by removing carotid plaque and unnarrowing the carotid artery, thereby increasing blood supply to the distal brain. At present, cerebral infarction has become a serious disease that endangers human health, and one of the important causes of cerebral infarction is carotid artery stenosis, that is, when the carotid artery, an important general valve, is severely narrow, the cerebral blood vessel of its distal blood flow is inevitably ischemic. Therefore, vigorously carrying out this work can benefit the majority of patients with carotid artery stenosis. In clinical practice, many patients are found to have carotid artery stenosis after physical examination or admission for other reasons. We strictly grasp the indications. In general, CEA can be used as a treatment option for more than 50% of stenosis, but there is no absolute thing in clinical practice, and surgical indications are flexible. For example, some patients have frequent TIA attacks, plaques accompanied by ulcers, and surgical treatment should be performed even if the stenosis does not reach 50%. The following is a recent operation performed by our cerebrovascular department.
Case Presentation
66-year-old female patient with "diabetes, metabolic syndrome" admitted to the endocrinology department. During routine admission physical examination, vascular ultrasound indicateded uneven thickening of the carotid intima on both sides with multiple plaques, right subclavian artery plaques, and severe carotid artery stenosis (70%-99%) on the left side. MRI-DWI revealed multiple acute cerebral infarctions in the left frontal parietal semi-oval center (Figure. 1). Carotid artery stenosis is closely related to cerebral watershed infarction (CWSI). In this case, it is shown that due to the stenosis of the extracranial segment of the carotid artery by more than 50% and the decrease of blood pressure, there will be hypoperfusion of the anterior cerebral artery (ACA) and the middle cerebral artery (MCA), resulting in CWSI.
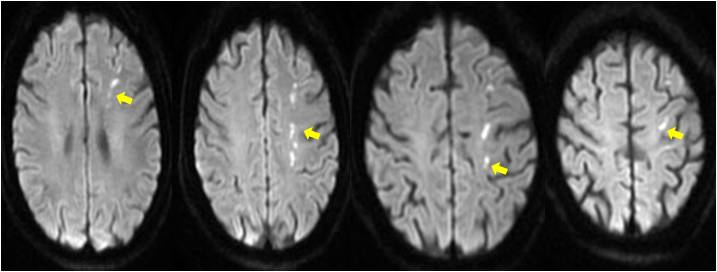
Figure. 1: MRI-DWI indicates multiple acute cerebral infarction in the left frontal parietal semi-oval center(Yellow arrow). Demonstrated CWSI in the LACA and MCA supply area。
In the process of examination, in addition to the serious complications of diabetes, the triglyceride level of the patient was also beyond the average level of normal people. After blood glucose stabilization in the endocrinology department, she was transferred to the cerebrovascular department to prepare for the treatment of severe carotid artery stenosis. Preoperative evaluation was completed in the cerebrovascular department: CTA indicated that the left common carotid artery (LCCA)met the CEA surgical treatment standard recommended by NASCET, that is, the stenosis was within the range of 70-99% (Figure 2-1, 2-2).
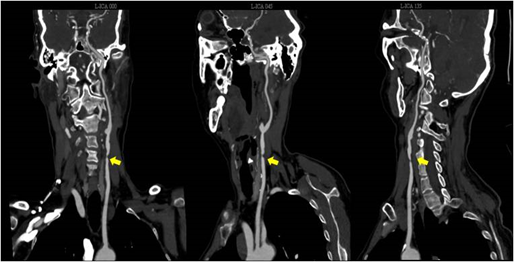
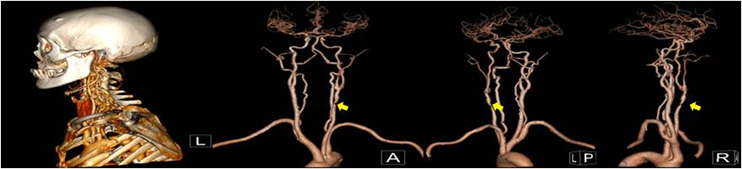
Figure. 2-1 2-2: CTA indicated that the LCCA met the CEA surgical treatment standard recommended by NASCET, that is, the stenosis was within the range of 70-99%(Yellow arrow.
In order to further clarify the surgical indications, the cerebrovascular department performed cerebrovascular angiography (DSA) on the patient, and the angiography results were completely consistent with the results suggested by CTA (Figure. 3). Moreover, CTP indicated that there was an obvious cerebral vascular deficiency area in the left carotid artery blood supply area compared with the right side (Figure. 4).
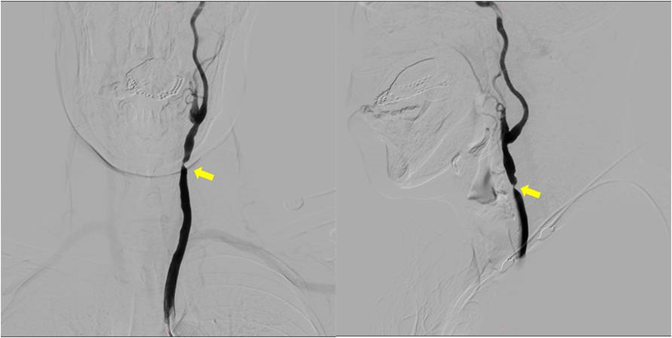
Figure 3: DSA showed severe stenosis of the LCCA. The stenosis was within the range of 70-99%(Yellow arrow), consistent with the results suggested by CTA.
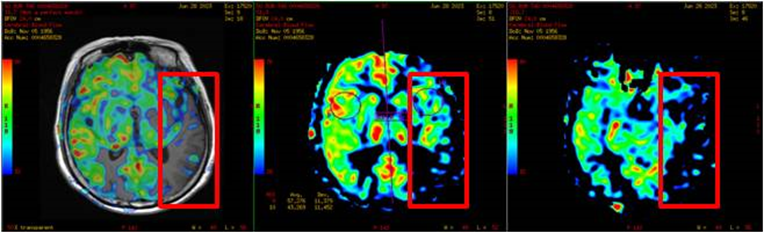
Figure. 4: CTP indicates that there is an obvious cerebral vascular deficiency in the left carotid artery blood supply area compared with the right. (The red box shows areas of low perfusion)
After completing all preoperative evaluations, considering that the patient had been diagnosed for more than one month and was in good condition with no obvious positive signs of nervous system after physical examination, we performed carotid artery dissection in strict accordance with Handbook of Neurosurgery, 8e [5] after completing the examination.
The basic procedure is as follows: After the obvious effect of general anesthesia, the supine position is taken. Tilt the head back slightly and rotate to the right side (Figure. 5). Routine disinfection and placement of sterile surgical towels. The incision at the anterior edge of the left sternocleidomastoid muscle was about 6cm long. The skin, subcutaneous, and platysma muscles were cut, and the carotid sheath was separated and exposed layer by layer along the anterior edge of the sternocleidomastoid muscle, and the common carotid artery(CCA) was separated and exposed by opening the carotid sheath (Figure. 5). Intravenous heparin 3000 units, blood vessel blocking clamp to block the common carotid artery, increase blood pressure. The longitudinal incision of the carotid artery under the microscope and the stripping of carotid plaque showed ulceration on the surface of the plaque, large lipid core, and calcification (Figure. 5). Heparin saline irrigation to remove free intimal debris. With 6-0 Proline suture, the common carotid artery was released after the carotid cavity was filled with heparin saline. No active bleeding was found. Hemostatic gauze was applied to the incision. Suture the carotid sheath and place an indwelling drainage tube outside the carotid sheath. Suture platysma muscle, subcutaneous, skin. After surgery, the patient was conscious and the tracheal tube was removed. Postoperative routine observation to ensure the safety and reliability of patients.

Figure. 5: Surgical position and removed atherosclerotic plaque. (Green arrows show the formation of ulcers within the plaque).
Discussion and summary:
It should be emphasized that in addition to routine examinations, CEA, especially special examinations, include echocardiography. In this case, the patient had atrial fibrillation, head MRI, cerebral perfusion and plaque stability, which require comprehensive examinations, such as CTA (DSA),CTP and carotid vascular high-resolution magnetic resonance imaging. Position, especially the neck should not be excessively twisted to cause cervical injury. Regarding the use of "double antibody" in the perioperative period, it should be adjusted according to the different taking habits of patients. During the operation, the anesthesiologist should ensure that the basic blood pressure level is increased by 20 mmHg before blocking and then restored after blocking. Instrument nurses should be familiar with specialized surgical instruments, and prepare all intraoperative instruments and drugs. The precautions of the surgeon during the operation will not be repeated this time. Here, it is especially explained that postoperative management and observation points, especially in the department nursing unit, should be frequent observation of changes in nerve function such as consciousness, pupil and limb movement, pay attention to pupil diameter and response to light, and take into account the possibility that cervical sympathetic ganglion stimulation may lead to Horner syndrome. The patency of CCA and external carotid artery (ECA) was evaluated by the pulse of superficial temporal artery. The activity of the tongue muscle, whether the Angle of the mouth is symmetrical, observe whether the incision is bleeding, swelling, tension, such as considering arterial hematoma, need to seek urgent medical treatment. Observe the patient's breathing, pay attention to laryngeal edema and so on.
Carotid ultrasound was reviewed every 3 months after surgery. Head and neck CTA was reviewed 3 months after surgery and every 1-2 years if no abnormalities were found. If there is also severe contralateral stenosis, surgery can be performed again after 6 months.
Conflict of Interest
The author has no financial conflicts of interest
References
- Ferguson GG, Eliasziw M, Barr HW, Clagett GP, Barnes RW, et al. (1999). The North American Symptomatic Carotid Endarterectomy Trial: Surgical results in 1415 patients. Stroke. 30: 1751-1758.
View at Publisher | View at Google Scholar - Warlow CP. (1993). Symptomatic patients: The European Carotid Surgery Trial (ECST). J Mal Vasc.18: 198-201.
View at Publisher | View at Google Scholar - Carotid surgery versus medical therapy in asymptomatic carotid stenosis. The CASANOVA Study Group. Stroke. 1991; 22: 1229-1235.
View at Publisher | View at Google Scholar - Rudarakanchana N, Dialynas M, Halliday A. (2009). Asymptomatic Carotid Surgery Trial-2 (ACST-2): rationale for a randomised clinical trial comparing carotid endarterectomy with carotid artery stenting in patients with asymptomatic carotid artery stenosis. Eur J Vasc Endovasc Surg.38: 239-242.
View at Publisher | View at Google Scholar - De Backer A. (2016). Handbook of neurosurgery, 8th edition. Acta Chir Belg.116: 269.
View at Publisher | View at Google Scholar

 Clinic
Clinic
